Season 1 of the Capability Corner podcast brought together Ausmed's Chief Customer Officer Michelle Wicky, Chief Nursing Officer Dr Karen Patterson, and Head of Learning and Capability Zoe Youl for candid, thought-provoking conversations about workforce development in healthcare. Across 10 episodes, several powerful themes emerged that are reshaping how we think about capability, compliance, and care.
Here are the seven biggest takeaways from the season, and what you should do differently in 2026 as a result.
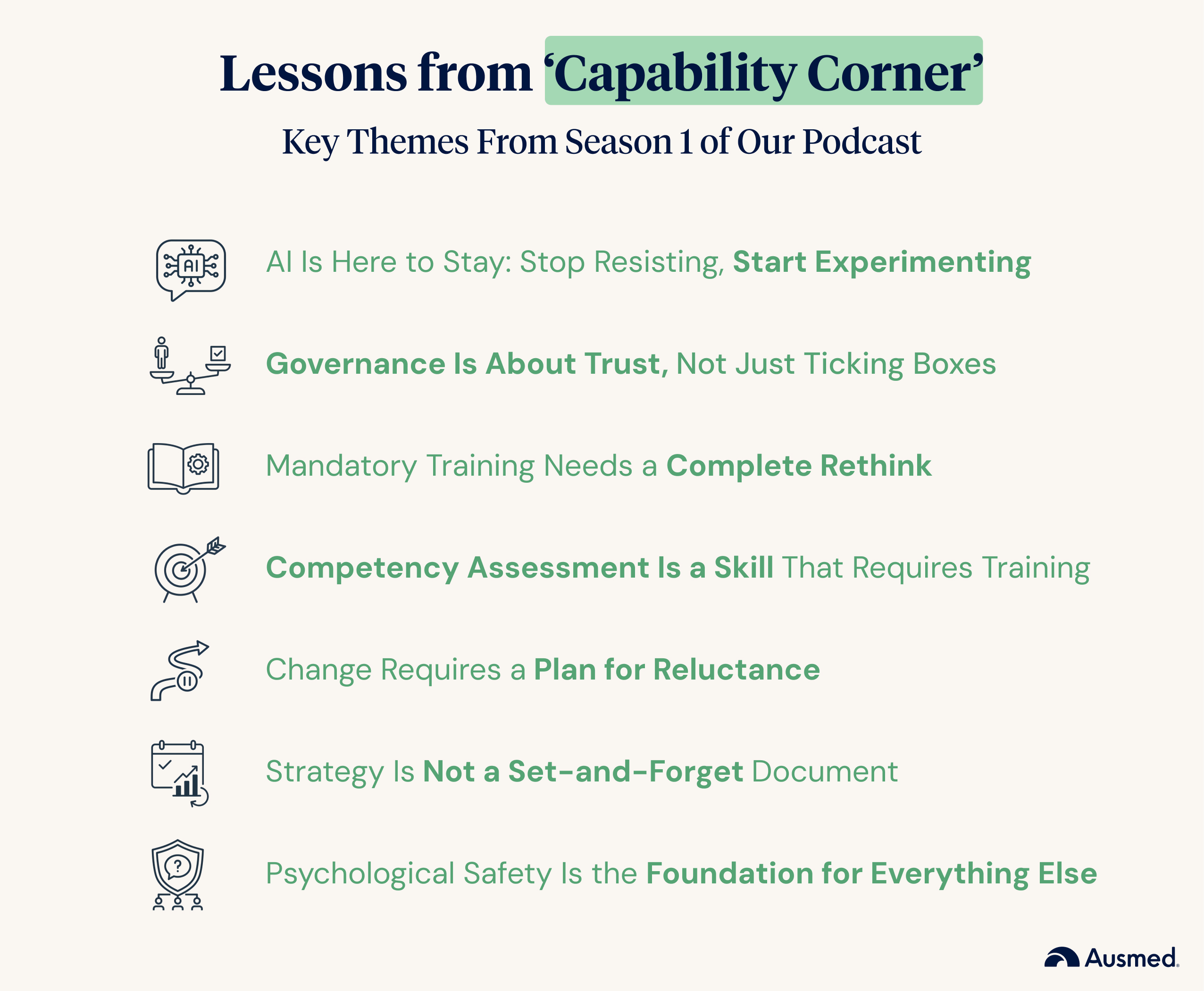
AI Is Here to Stay: Stop Resisting, Start Experimenting
If there was one message that echoed throughout the season, it was this: the wilful resistance to generative AI needs to end. Michelle didn't mince words in her opening rant, comparing AI reluctance to "clutching clipboards like I'm trying to replace their firstborn child."
The hosts dedicated multiple episodes to unpacking both the opportunities and governance considerations around AI. As CEO Will Egan put it when joining as a guest in Episode 7: AI Risks & Opportunities, AI represents a shift toward "generative learning", moving from static content to dynamic, contextualised experiences where learners receive real-time coaching and feedback.
What to do differently in 2026:
- Stop waiting for a mandate. If you haven't experimented with AI tools yet, start now. Use ChatGPT to draft documentation, summarise meeting notes, or build training outlines.
- Build AI into your capability strategy. As explored in Episode 8: AI Generative Learning & Governance, consider how AI can augment workflows while freeing up time for higher-value work.
- Advocate for governance, not avoidance. Push for clear AI policies in your organisation so people feel safe to experiment within defined guardrails.
Governance Is About Trust, Not Just Ticking Boxes
When the topic of governance arose in Episode 6, Dr Karen Patterson reframed it in an unexpectedly relatable way, comparing it to hosting a family gathering. "Your job is to make sure the oven's working, there's enough chairs for everyone, and that Uncle Joe doesn't try to deep fry the turkey inside," she explained. "When you do your job well, the family can relax and enjoy."
This metaphor captured the essence of effective governance: it's not about control, it's about creating conditions where people feel safe, supported, and able to deliver their best work.
What to do differently in 2026:
- Reframe governance conversations. Move away from "compliance and control" language toward "trust and enablement." Ask: what conditions do our people need to do their best work?
- Make governance visible and human. Bring governance out of policy documents and into everyday conversations. Explain the why behind the rules.
- Use governance to enable, not restrict. As Zoe summarised: "Compliance is doing the bare minimum. Governance is about capability." Design frameworks that support growth, not just risk mitigation.
Mandatory Training Needs a Complete Rethink
Few topics sparked as much passionate discussion as mandatory training. The hosts were united in their frustration with what Michelle called "checkbox culture", the belief that completion equals competence. Episode 2: Ticked Off? Debating Mandatory Training tackled this head-on.
The problem, as they unpacked it, isn't education itself. It's the approach. Annual refreshers disconnected from actual practice, training that fails to account for the specific needs of different roles and care contexts, and a regulatory focus on completion metrics rather than outcomes, all came under fire.
What to do differently in 2026:
- Audit your mandatory training plan. Ask: is this training still relevant? Does it address actual risks in our context? Could it be replaced with a competency verification instead?
- Move from time-based to outcome-based. Instead of asking "Have they completed the training?", ask "Can they demonstrate the capability in practice?"
- Tailor training to role and context. Map training requirements to specific job roles and the prevalent needs of the people in your care, rather than applying a one-size-fits-all approach.
Competency Assessment Is a Skill That Requires Training
One of the season's most pointed rants in Episode 3: The Competency Conversation addressed a common but problematic practice: delegating competency assessments to anyone with a clipboard and a pulse. "Just because you can give an injection doesn't mean you can assess an injection," Michelle declared.
The hosts explored the four principles of assessment (fair, flexible, valid, and reliable) and highlighted that assessing competence is itself a regulated, structured skill. When assessors don't understand these principles, the entire foundation of competency-based education crumbles.
What to do differently in 2026:
- Invest in assessor training. Don't assume that clinical expertise equals assessment expertise. Provide formal training on the four principles of assessment.
- Review your verification methods. Are you using the right method for the competency being assessed? Direct observation, simulation, and written evidence all have different applications.
- Build assessment capability across your team. Make competency assessment a core skill for anyone in a supervisory or education role, not just an afterthought.
Change Requires a Plan for Reluctance, Not Just a Plan for Change
Episode 4: Why Is Change So Messy? tackled change management with a twist. Rather than focusing on the typical change management playbook, the hosts argued for adding something new: a change reluctance plan.
This isn't about forcing people to change. It's about acknowledging that resistance is normal and building support structures for those who are struggling. Karen introduced Lewin's change model and the concept of "sludge", acknowledging that change is messy and the new state needs to constantly evolve.
What to do differently in 2026:
- Add a "reluctance layer" to your change plans. Identify where people might be on the spectrum from reluctance to resistance, and plan tailored support for each stage.
- Name resistance without shame. Create space for people to voice their concerns. Resistance often signals unmet needs or unaddressed fears.
- Build in continuous revisiting. Change isn't a one-time event. Schedule regular check-ins to assess how the change is landing and adapt your approach accordingly.
Strategy Is Not a Set-and-Forget Document
When Zoe shared her experience developing new content strategy in Episode 5: Strategy Is Shared Language, it opened a broader conversation about how organisations treat strategic planning. Too often, Michelle observed, strategy documents become "like a dying business plan of a sole trader", written with good intentions, then shoved in a drawer and forgotten.
The hosts argued that strategy needs to be a living, breathing part of daily operations. It requires continuous revisiting, transparent communication about progress, and the courage to pivot when circumstances change.
What to do differently in 2026:
- Put strategy reviews in your calendar. Schedule monthly or quarterly check-ins to ask: are we still on track? Does this strategy still make sense given what's changed?
- Talk about strategy regularly. Reference it in team meetings, use it to frame decisions, and celebrate progress that aligns with strategic goals.
- Be willing to pivot. As Karen noted, if all the signals are telling you to change direction, don't cling to a five-year plan that's no longer fit for purpose. Strategy should serve outcomes, not the other way around.
Psychological Safety Is the Foundation for Everything Else
Running beneath every conversation this season was an implicit theme: psychological safety. Whether discussing governance, performance management in Episode 9, AI adoption, or change, the ability for people to feel safe enough to speak up, make mistakes, and grow emerged as the critical enabler.
Karen noted that mandatory training approaches can actually erode trust between staff and leadership when they become punitive or disconnected from reality. Emma Piercy, joining as a guest to discuss performance management, highlighted that "if people feel safe to speak up, you can catch risks before they escalate into incidents, complaints, or Fair Work cases."
The bonus episode on Psychological Safety with Rasa Kabaila NP dove deeper into what this looks like in practice.
What to do differently in 2026:
- Assess your team's psychological safety. Ask: do people feel safe to speak up, ask questions, and admit mistakes? If not, what's getting in the way?
- Model vulnerability as a leader. Share your own learning edges and mistakes. This signals that growth, not perfection, is the expectation.
- Connect psychological safety to business outcomes. Frame it not as a "nice to have" but as a risk mitigation strategy. Safe teams catch problems earlier, retain staff longer, and deliver better care.
Looking Ahead
As Capability Corner wrapped its first season, our hosts reflected on a year of significant change in healthcare, from the implementation of the strengthened aged care standards to the rapid emergence of generative AI. But their message remained consistent: capability building is about more than compliance, and the organisations that thrive will be those that embrace change, invest in their people, and build cultures of trust and continuous learning.
These seven themes offer a practical framework for any healthcare leader looking to build a more capable, resilient workforce in 2026 and beyond.
Ready to dive deeper? Listen to all episodes of the Capability Corner wherever you get your podcasts, and subscribe to the Ausmed Toolbox for articles, resources, and practical guides on workforce capability.



