Did you know that cataracts are the leading cause of blindness worldwide among adults (Healthdirect 2021)?
What are Cataracts?
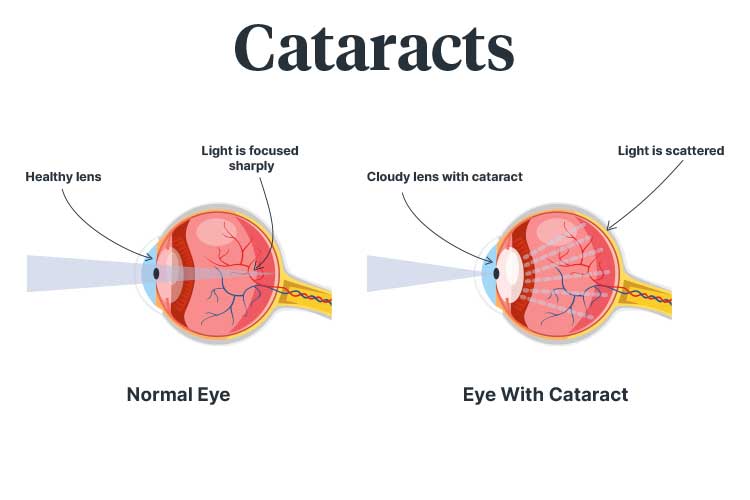
The human eye is made up of several components used to receive and transmit visual information (Davson & Perkins 2023). The lens, which sits behind the iris, plays an important role in focusing light on the retina, a light-sensitive membrane at the back of the eye. The light that hits the retina is turned into electrical signals that are transmitted through the optic nerve to the brain (NEI 2022; Mayo Clinic 2023).
The lens in a healthy eye should be clear, allowing the retina to receive a clear, sharp image (Mayo Clinic 2023). A cataract is when the lens becomes cloudy, causing vision impairment (Vision Australia 2017).
Cataracts are primarily age-related. In fact, almost every person who is 70 or older has some level of cataract formation (Better Health Channel 2023).
Despite this, it is possible, albeit less common, for people to develop cataracts at a young age or even be born with them (Vision Australia 2017).
Cataracts may be unilateral (affecting one eye) or bilateral (affecting both eyes) (Healthdirect 2021).
Luckily, while cataracts are a leading cause of blindness, most people can be successfully treated and regain their vision (Healthdirect 2021).
What Causes Cataracts?
The lenses in the eyes generally become less flexible, thicker and less transparent over time. With age or certain conditions, proteins and fibres in the lenses break down and form clumps. These clumps cloud areas of the lens, creating cataracts. The clouding gradually expands and becomes more dense (Mayo Clinic 2023; NEI 2023).
Cataract Statistics in Australia
Cataracts are estimated to affect around 411,000 Australians (AIHW 2021).
In Australia, cataracts are the second most common cause of bilateral vision impairment (Croakey Professional Services 2022) and cataract surgery is the most common elective surgical procedure (ACSQHC 2021).
Cataracts are a significant issue for Aboriginal and Torres Strait Islander people, being 12 times more likely to affect First Nations people than non-First Nations Australians. Furthermore, First Nations people wait about 63% longer than non-First Nations Australians to receive cataract surgery (Vision 2020 Australia 2019).
Types of Cataracts
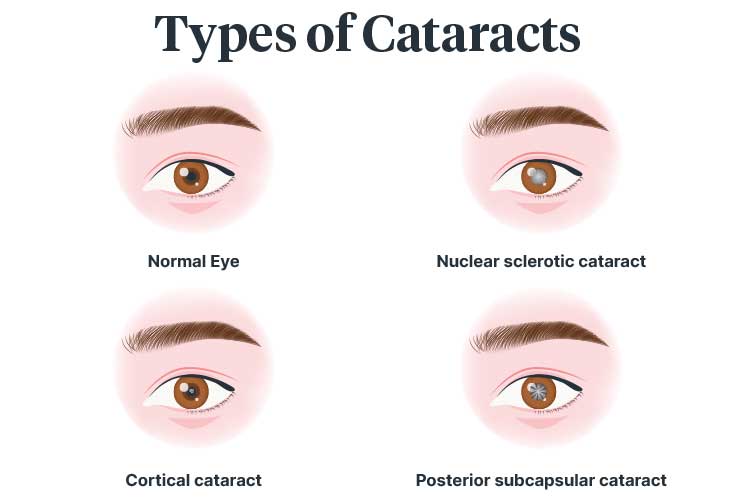
Cataracts can be categorised depending on their location within the lens:
- Nuclear sclerotic cataracts develop over time as the nucleus (centre) of the lens hardens and becomes yellow. They are the most common type of cataract and progress gradually. They generally affect focus and, in some cases, may cause a temporary improvement in close-up vision.
- Cortical cataracts are less common, affecting the cortex (peripheral outer part) of the lens. Cortical cataracts are fissures that resemble the spokes of a wheel, pointing inwards to the middle of the lens. These fissures cause light to scatter when hitting the retina, often causing issues with glare.
- Posterior subcapsular cataracts occur on the back surface of the lens, under the lens capsule. They often cause reading issues, light sensitivity, glare and ‘halo’ effects. Posterior subcapsular cataracts generally progress the most quickly and are more likely to affect people with diabetes or those with prolonged corticosteroid use.
(Vision Eye Institute 2017; Mayo Clinic 2023)
Congenital cataracts may be related to genetics, intrauterine infection, trauma or conditions such as rubella (Mayo Clinic 2023).
Risk Factors for Cataracts
In addition to age, other risk factors include:
- Family history of cataracts
- Diabetes
- Eye injury
- Unprotected eye exposure to sunlight over a long period of time
- Long-term smoking
- Long-term corticosteroid use.
(Vision Australia 2017; Healthdirect 2021)
Symptoms of Cataracts
Someone with cataracts may experience:
- Blurry, hazy or foggy vision
- Sensitivity to glare
- Double vision
- Distorted vision
- Colours appearing faded or yellowed
- ‘Halo’ effects around lights
- The feeling that they are looking through a curtain or veil
- Frequent prescription changes for corrective lenses
- Difficulty reading, driving at night, seeing faces or noticing details.
(Vision Australia 2017; Healthdirect 2021; Mayo Clinic 2023)
Symptoms may not be noticeable until the cataract has progressed to a more advanced stage (Vision Australia 2017).
Diagnosing Cataracts
Cataracts can be identified through an eye examination, where a practitioner will assess vision, the appearance of the eye and the retina. The pupils may need to be dilated using eye drops so that the retina can be examined. A slit lamp may be used to magnify the eye so that the location and pattern of the cataract can be determined (Healthdirect 2021; Mayo Clinic 2023).
Other tests, such as a CT scan, MRI scan or ultrasound, may be used to examine the back of the eye (Healthdirect 2021).
Treatment for Cataracts
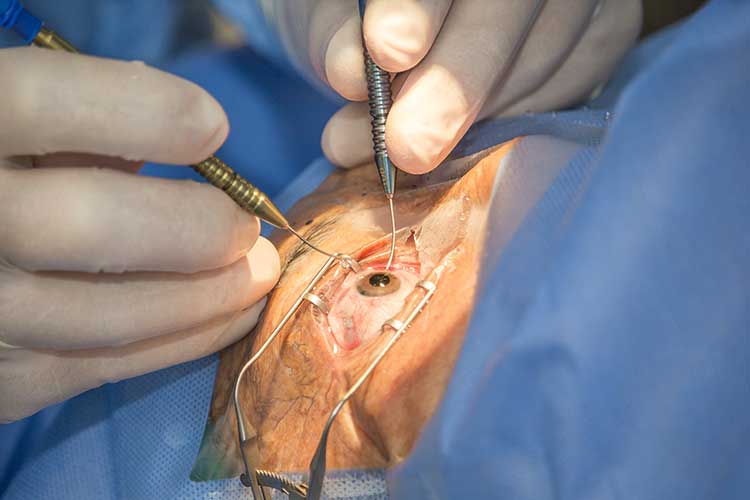
Glasses and visual aids such as magnification and lighting modifications may improve vision in the early stages of a cataract, but these are not permanent solutions. Once the cataract progresses, surgical treatment is the only effective long-term option (Vision Australia 2017; Healthdirect 2021).
Cataract surgery is one of the most commonly performed and successful surgical procedures (Vision Australia 2017). It is straightforward and performed in about 30 minutes, generally only requiring local anesthetic (Healthdirect 2021).
The procedure involves removing the clouded lens and replacing it with a new, artificial one (Healthdirect 2021).
Replacing the affected lens with an artificial one may also correct any refractive errors (such as myopia). As a result, some patients may no longer require glasses after the procedure (Kelley 2021).
Preventing Cataracts
The risk of cataracts may be reduced by:
- Wearing a hat and sunglasses outside to protect the eyes from the sun
- Smoking cessation
- Regular eye examinations
- Seeking advice from a health professional if vision changes occur.
(Vision 2020 Australia 2018)
The Cataract Clinical Care Standard
The Cataract Clinical Care Standard was released by the Australian Commission on Safety and Quality in Health Care in 2021.
This standard aims to guide the assessment and care of patients over the age of 18 with cataracts in all healthcare settings (ACSQHC 2021).
The standard comprises the following eight Quality Statements:
| Quality Statement 1: Primary care assessment and referral | Patients with suspected cataracts undergo an initial assessment for:
|
| Quality Statement 2: Patient information and shared decision-making | Patients are provided information in a form that is appropriate for them to support shared decision-making. They are given the opportunity to discuss their needs and preferences, as well as the potential benefits and consequences of their options. |
| Quality Statement 3: Access to ophthalmology assessment | Patients who have been referred for surgery consideration are prioritised for ophthalmology assessment based on their clinical needs. |
| Quality Statement 4: Indications for cataract surgery | Patients are offered surgery when their cataracts are at a stage where:
|
| Quality Statement 5: Prioritisation for cataract surgery | Patients are prioritised for surgery based on:
|
| Quality Statement 6: Second-eye surgery | When a patient with bilateral cataracts is planning surgery for their first eye, the practitioner should discuss with the patient whether the second eye will be operated on and, if so, when the second procedure will take place. |
| Quality Statement 7: Preventive eye medicines | Patients should receive an intracameral antibiotic injection at the time of surgery. Postoperatively, they should receive anti-inflammatory eye drops only if indicated. |
| Quality Statement 8: Postoperative care | Patients should receive appropriate postoperative care until they have recovered to ensure any complications are addressed. |
(ACSQHC 2021)
Test Your Knowledge
Question 1 of 3
What type of cataract is characterised by fissures resembling a wheel's spokes?
Topics
References
- Australian Commission on Safety and Quality in Health Care 2021, Cataract Clinical Care Standard, Australian Government, viewed 24 January 2024, https://www.safetyandquality.gov.au/publications-and-resources/resource-library/cataract-clinical-care-standard-2021
- Australian Institute of Health and Welfare 2021, Eye Health, Australian Government, viewed 24 January 2024, https://www.aihw.gov.au/reports/eye-health/eye-health/contents/new
- Better Health Channel 2023, Cataracts, Victoria State Government, viewed 23 January 2024, https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/cataracts
- Croakey Professional Services 2022, ‘New Standard Outlines a Vision for Safety, Quality and Equity in Cataract Care’, Australian Commission on Safety and Quality in Health Care Newsroom, 8 March, viewed 24 January 2024, https://www.safetyandquality.gov.au/newsroom/external-publications/new-standard-outlines-vision-safety-quality-and-equity-cataract-care
- Davson, H & Perkins, ES 2023, ‘Human Eye’, Encyclopaedia Britannica, viewed 23 January 2024, https://www.britannica.com/science/human-eye
- Healthdirect 2021, Cataracts, Australian Government, viewed 23 January 2024, https://www.healthdirect.gov.au/cataracts
- Kelley, S 2021, What is Refractive Cataract Surgery?, All About Vision, viewed 24 January 2024, https://www.allaboutvision.com/eye-surgery/cataract-surgery/faq-refractive-cataract-surgery
- Mayo Clinic 2023, Cataracts, Mayo Clinic, viewed 23 January 2024, https://www.mayoclinic.org/diseases-conditions/cataracts/symptoms-causes/syc-20353790
- National Eye Institute 2023, Cataracts, U.S. Department of Health & Human Services, viewed 24 January 2024, https://www.nei.nih.gov/learn-about-eye-health/eye-conditions-and-diseases/cataracts
- National Eye Institute 2022, How the Eyes Work, U.S. Department of Health & Human Services, viewed 23 January 2024, https://www.nei.nih.gov/learn-about-eye-health/healthy-vision/how-eyes-work
- Vision 2020 Australia 2018, Info Sheet: Cataracts, Vision 2020 Australia, viewed 24 January 2024, https://www.visioninitiative.org.au/uploads/assets/files/infosheets/2017_CAT_Eng_vi-factsheet-cataracts-final.pdf
- Vision 2020 Australia 2019, Strong Eyes, Strong Communities: A Five Year Plan for Aboriginal and Torres Strait Islander Eye Health and Vision, Vision 2020 Australia, viewed 23 January 2024, https://www.vision2020australia.org.au/wp-content/uploads/2019/03/Strong-Eyes-Strong-Communities-A-five-year-plan-for-Aboriginal-and-Torres-Strait-Islander-eye-health-and-vision-2019-2024.pdf
- Vision Australia 2017, Cataracts, Vision Australia, viewed 23 January 2024, https://www.visionaustralia.org/information/eye-conditions/cataracts
 New
New 
