'I feel so tired, all the time. And the pain… sometimes I have pain in my leg that’s so bad I can’t walk and just to touch it… it feels like someone has slammed into it with a hammer. I have trouble sleeping, I have trouble concentrating… and did I mention the tiredness? When I’m stressed the pain becomes worse, and it’s not only in my leg, sometimes it feels like I have it everywhere, but the leg is always the worst.'
– Quoted from Ms X
You are probably wondering what has happened to Ms X. What is the cause of this pain?
Is the pain causing the fatigue and difficulty concentrating, or is the fatigue making the pain worse?
Why is the pain worse when she is stressed?
And why is it widespread and not just affecting her leg?
For people with fibromyalgia, a condition that often severely impacts quality of life, these questions can not always be answered.
What is Fibromyalgia?
Fibromyalgia is a musculoskeletal pain syndrome with no clearly identified cause. Due to this, treatment tends to be difficult. Fibromyalgia is estimated to affect 2 to 5% of the population and is more common in women than men (Healthdirect 2023).
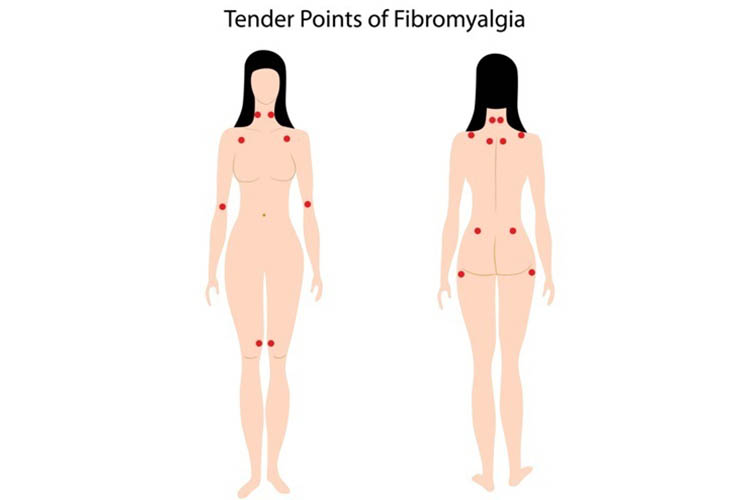
The most debilitating symptom of this condition is chronic and widespread pain (Healthdirect 2023). Fibromyalgia may also cause a neurological symptom called allodynia, which affects the body’s perception of pain. This means the brain will interpret harmless stimuli as painful, leading to increased sensitivity that causes the slightest touch to feel extremely painful (He & Kim 2022).
Other symptoms may include:
- Increased sensitivity to temperature, light, smell and noise
- Chronic fatigue
- Sleep problems
- Concentration and memory issues
- Anxiety and/or depression
- Irritable bowel syndrome
- Headaches
- Numbness and tingling in arms and legs
- Restless legs
- Painful menstrual periods.
(Healthdirect 2023; Better Health Channel 2019)
Diagnosing Fibromyalgia
Fibromyalgia is difficult to diagnose as there is no specific diagnostic test available (Healthdirect 2023).
Instead, diagnosis is based on patient history, physical examination, and blood tests in order to rule out other potential causes and diagnose any comorbid conditions (Fibromyalgia Australia 2020).
This diagnostic process may involve:
- Patient history of widespread pain over time
- Is the onset abrupt or gradual, or is it related to a particular illness or event?
- Is it stable, improving or worsening over time?
- How long does it last for, and is there a daily pattern?
- Are there any factors that improve or worsen the pain?
- What impact doed the pain have on the patient’s daily ife? Have they needed to make adjustments to their routine due to the pain?
- The patient may need to undergo tests to exclude other conditions that may explain their symptoms.
- Physical examination of musculoskeletal and neurological changes, including muscle weakness, neurological signs and/or other symptoms that may suggest an overlapping condition. Assess for:
- Lymphadenopathy, thyroid disease, cardiac or pulmonary disease, joint or connective tissue disease
- Diffuse tenderness in soft tissues
- Lying and standing blood pressures
- Treatable areas such as sleep disorders, underlying arthritic inflammatory conditions, depression or anxiety, gut prolems and other primary pain conditions.
- Investigations
- Routine blood tests to rule out other diagnoses or comorbidities:
- FBC, CRP, ferritin, creatinine
- Electrolytes, renal and liver function, calcium, magnesium
- Fasting blood glucose and insulin
- Thyroid function and antibodies (TSH, T3, T4)
- B12, folate, vitamin D
- Iron Studies
- Urinalysis
- Other tests that are clinically indicated.
- Routine blood tests to rule out other diagnoses or comorbidities:
- Referral to specialistss - only required if:
- There is considerable uncertainty about the patient’s diagnosis
- Symptoms indicate an underlying or overlapping condition
- Further ongoing assessments.
(Fibromyalgia Australia 2020)
Treatment of Fibromyalgia
Unfortunately, there is no specific cure for fibromyalgia. Treatment focuses on symptom control and pain management.
Treatment will often take a multimodal approach and incorporate strategies such as:
- Patient education
- Exercise
- Pain management
- Stress management
- Maintaining a balance of rest and activity
- Cognitive behaviour therapy (CBT)
- Staying at work
- Sleep
- Massages
- Mindfulness
- Transcutaneous electrical nerve stimulation (TENS)
- Acupuncture
- Maintaining a healthy, well-balanced diet
- Attending peer support groups
- Medications.
(Better Health Channel 2019)
Pain Management for Fibromyalgia

The pain experienced from fibromyalgia is often difficult to manage, partially because it is understood to originate from the brain rather than the muscles and bones (Healthdirect 2023).
One theory is that people with fibromyalgia have experienced a change in the way their central nervous system processes pain, causing increased sensitivity. Fibromyalgia may also be associated with abnormal levels of certain neurotransmitters (NHS 2022).
Pharmacological pain management may include analgesics, antidepressants and anticonvulsants (Better Health Channel 2019).
Often, treatment will be holistic and involve a variety of interventions to ensure the patient is cared for in all aspects of their health, as fibromyalgia can affect all areas of an individual’s life.
Every person with fibromyalgia will have different symptoms and different treatment goals, so treatment is individualised.
As nurses, we may find our role is to provide support to the individual, as well as focus on pain management.
It is also important to remember that fibromyalgia isn’t only about pain management - there are many other symptoms the patient will be experiencing, and all of these symptoms will be impacting on their quality of life.
Considerations When Designing Exercise Programs for Patients with Fibromyalgia
Helping patients with fibromyalgia keep active is one of the most useful ways to manage their symptoms. When designing a program for individuals with fibromyalgia, it is useful to first consider some of the more common issues that arise with this population.-
Fatigue
For a patient with fibromyalgia, fatigue, like pain, is a constant concern. Individuals who act as weekend warriors and give their all during therapy may end up unable to participate in daily life post-exercise.
-
Depression and social isolation
Fibromyalgia has a significant impact on social interaction and mood. Individualised sessions of one-to-one therapy may not address the root of this concern: the need for peers who understand and can commiserate with each other. Consider enrolling patients in group classes instead of one-to-one therapy; this is especially useful if the group class has a strong social component.
-
Need for predictability
Individuals with fibromyalgia can become dependent on ritualised behaviours to the extent of presenting with anxiety when these rituals are disturbed. Therapists who routinely add novelty to treatment sessions may engender a sense of quiet desperation in patients who simply long for a reliable level of training intensity.
-
Hypersensitivity to Pain
Patients with fibromyalgia often present with strong pain sensitivities and they may overreact to the sensory overload present during exercise sessions.
Patients with fibromyalgia need to exercise and they need to do so consistently. Aquatic exercise in warm water is often suggested as the perfect solution for this population. Because an aquatic environment makes it possible for individuals to move easily without being bombarded with pain, patients may be willing to move in ways they would never (and should never) attempt on land.
With exercise, a cycle of movement freedom can be birthed and then reared into something sustainable.
Conclusion
Every person with fibromyalgia will have different symptoms and different treatment goals, so treatment is individualised.
As nurses, we may find our role is to provide support to the individual, as well as focus on pain management.
It is also important to remember that fibromyalgia isn’t only about pain management - there are many other symptoms the patient will be experiencing, and all of these symptoms will be impacting on their quality of life.
Test Your Knowledge
Question 1 of 3
True or false: Fibromyalgia is more common in women than men.
Topics
References
- Better Health Channel 2019, Fibromyalgia, Victoria State Government, viewed 1 June 2023, https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/fibromyalgia
- Fibromyalgia Australia 2020, Fibromyalgia Understanding the Diagnosis and Assessments, Bridges & Pathways Institute, viewed 2 June 2023, https://fibromyalgiaaustralia.org.au/wp-content/uploads/Patient-Leaflet-04-Fibromyalgia-Understanding-Your-Diagnosis.pdf
- Healthdirect 2023, Fibromyalgia, Australian Government, viewed 1 June 2023, https://www.healthdirect.gov.au/fibromyalgia
- He, Y & Kim, PY 2022, ‘Allodynia’, StatPearls, viewed 1 June 2023, https://www.ncbi.nlm.nih.gov/books/NBK537129/
- National Health Service 2022, Fibromyalgia, NHS, viewed 2 June 2023, https://www.nhs.uk/conditions/fibromyalgia/
 New
New 
