This article will provide a refresher on how to monitor, empty and change drainage bags for a client with a urinary catheter in-situ.
For information related to the catheterisation procedure, read: Caring For a Urinary Catheter.
Catheter Monitoring and Routine Care
As part of routine care, you should ensure that:
- There are no kinks or loops in the drainage bag tubing and the urine is being continuously drained
- Both the catheter and draining device are connected securely
- The drainage bag is supported by a stand or hook so that the outlet and tubing are kept off the floor
- The drainage bag is below bladder level at all times, including during transportation and when ambulating
- The catheter is attached to the person with a securing device
- The drainage device is closed unless it is being emptied.
(NSW Health 2021)
How to Empty the Catheter Drainage Bag
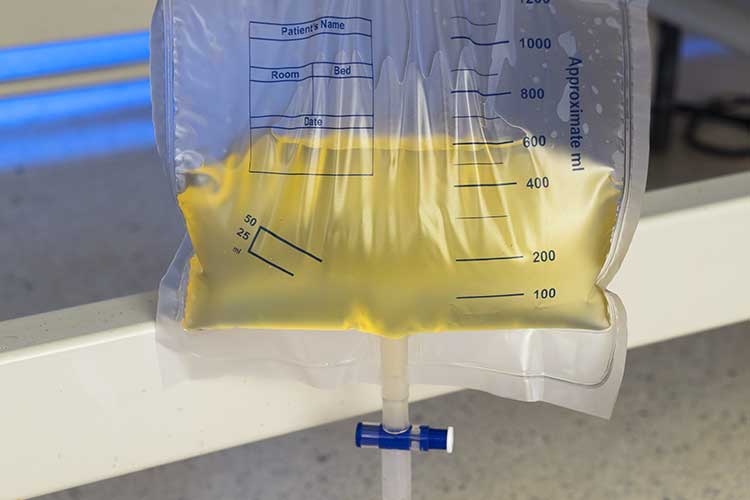
Drainage bags should be emptied when ¾ full and before any client transportation (NSW Health 2021).
- Explain the procedure to the person and gain consent.
- Ask the person whether they have been experiencing any issues with their catheter.
- Document the amount of urine that is in the bag.
- Perform hand hygiene.
- Gather required equipment.
- Ensure the person's privacy.
- Don appropriate PPE.
- Put the drainage bag over the device in which the draining will occur (clean receptacle or toilet).
- Open the port at the bottom of the drainage bag.
- Empty the bag into the toilet or clean receptacle (do not allow the drainage port to touch the toilet rim or receptacle). Note whether there is any unusual colour or smell to the urine.
- After the drainage bag has been emptied, dry the drainage port with a clean tissue or toilet paper.
- Close the drainage port.
- If using a receptacle, wash and dry it thoroughly.
- Perform hand hygiene.
(QSCIS 2020)
When to Change the Catheter Drainage Bag
The drainage bag should only be changed:
- At least every seven days as a general rule (note that changing the drainage bag too frequently can increase the risk of infection)
- In accordance with the manufacturer’s instructions
- If the drainage bag becomes disconnected from the catheter
- If the drainage bag tube is blocked due to a build-up of sediment
- If the drainage bag fails.
(NSW Health 2021)
How to Change the Catheter Drainage Bag
Remember to always use aseptic technique when changing a drainage bag (NSW Health 2021).
- Explain the procedure to the person and gain consent.
- Ask the person whether they have been experiencing any issues with their catheter.
- Document the amount of urine that is in the bag.
- Perform hand hygiene.
- Gather required equipment.
- Ensure the person's privacy.
- Don appropriate PPE.
- Put the drainage bag over the device in which the draining will occur (clean receptacle or toilet)
- Open the port at the bottom of the drainage bag
- Empty the bag into the toilet or clean receptacle (do not allow the drainage port to touch the toilet rim or receptacle). Note whether there is any unusual colour or smell to the urine.
- Put a protective sheet under the area where the catheter connects to the drainage bag.
- Hold the catheter firmly and twist the drainage bag to disconnect it. Ensure the bag does not touch the tip of the catheter.
- Place the old drainage bag into the appropriate waste receptacle for bodily fluids (follow your organisation’s policy).
- Clean the catheter lumen with an alcohol wipe and allow it to dry.
- Remove the plastic cap from the tubing of the new drainage bag - ensure you don’t touch the tip of the tube.
- Attach the new drainage bag to the catheter.
- Ensure the outlet on the new drainage bag is closed.
- If using a leg bag assist the client to fit it comfortably.
- Doff PPE and dispose of it appropriately.
- Perform hand hygiene.
- Document necessary information.
(NSW Health 2021)
When to Escalate Care
The following signs and symptoms may indicate a deterioration in the client’s health or a problem with the catheter and require immediate escalation of care to an appropriately qualified medical practitioner:
- Bladder cramps
- Cloudy, bloody, discoloured or unpleasant-smelling urine
- Fever, chills, shaking or generally feeling unwell
- Nausea or vomiting
- Pain in the bladder, pelvis, lower back or flank
- Irritation, swelling, redness or tenderness around the insertion site
- Lack of drainage from the catheter
- Leaking around the catheter
- Dislodgement of the catheter.
(Patient Info 2021)
Catheter Troubleshooting
If there is no drainage from the catheter:
- Check whether the catheter tubing is bent or kinked
- Ensure the drainage bag is below the client’s bladder level
- Check whether there is any sediment blocking the tubing
- Check whether the client has been drinking enough
- Ask the client to try moving around to see if it dislodges the blockage
- Contact an appropriately qualified medical practitioner if no urine has been passed after four hours.
(Patient Info 2021)

Infection Control
It is crucial to ensure proper infection control when attending to a urinary catheter:
- In order to uphold aseptic technique principles:
- Make sure the person's body is clean
- Use sterile equipment
- Always perform hand hygiene before and after attending to a catheter or performing catheter care
- Never lay a drainage bag on the floor while in use, as this increases the risk of infection
- Use separate receptacles for different clients
- The drainage port should never make contact with the receptacle or the toilet
- Ensure you change the drainage bag if it is discoloured, smells unpleasant, contains sediment or is damaged. Notify the medical team of these observations prior to changing the bag
- Note that changing the drainage bag too frequently will break the sterile system and increase the risk of infection
- Ensure drainage bags are changed at least every seven days
- Never reuse, wash or reconnect drainage bags
- Never add antiseptic or antimicrobial solutions to drainage bags
- Ask for help if needed.
(RCN 2021; Patient Info 2021)
Waste Management
Always dispose of waste, including used drainage bags, according to local policies and procedures (NSW Health 2021).
Note: This article is intended as a guide only for non-clinical staff providing catheter care to home care clients and should not replace best-practice care. Always refer to your organisation's policies and procedures on urinary catheter care, monitoring and drainage bag changes.
Test Your Knowledge
Question 1 of 3
At what volume should urine drainage bags be emptied?
Topics
References
- NSW Health 2021, Insertion and Management of Urethral Catheters for Adult Patients, New South Wales Government, viewed 12 March 2025, https://www1.health.nsw.gov.au/pds/Pages/doc.aspx?dn=GL2021_015
- Patient Info 2021, Home Management of Your Catheter, Hunter New England Local Health District, viewed 12 March 2025, https://ccpatientinfo.org.au/patientinfo/HNEHomeManagementOfYourCatheter.pdf
- Queensland Spinal Cord Injuries Service 2020, Caring for and Changing your Supra-Pubic Catheter (SPC), Queensland Government, viewed 12 March 2025, https://www.health.qld.gov.au/__data/assets/pdf_file/0024/422619/spc-care.pdf
- Royal College of Nursing 2021, Catheter Care: Guidance for Health Care Professionals, RCN, viewed 12 March 2025, https://www.rcn.org.uk/Professional-Development/publications/catheter-care-guidance-for-health-care-professionals-uk-pub-009-915
 New
New