Donning (putting on) and doffing (removing) personal protective equipment (PPE) is a critical process that requires significant care in order to limit exposure to pathogens.
Healthcare organisations should uphold appropriate infection control and prevention measures as per the National Safety and Quality Health Service Standards, Standard 3: Preventing and Controlling Infections.
What is Personal Protective Equipment?
The term personal protective equipment refers to any clothing or equipment used for protection (Safe Work NSW 2020).
In healthcare settings, PPE is used to create a barrier between you and any infectious agents that you may come into contact with during your work. The aim of this is to reduce the risk of touching, transmitting or being exposed to pathogens (MedlinePlus 2023).

PPE includes:
- Clothing (gowns, aprons, head covering and shoe covers)
- Gloves
- Masks (surgical or particle filter respirator)
- Eye protection (face shields and goggles).
(MedlinePlus 2023)
Using PPE Effectively
- Healthcare workers must be thoroughly informed about any infections and updated on the current policies, procedures and protocols of their organisation
- Workers must have access to the necessary equipment to carry out the specified task correctly and safely
- You may consider having a second clinician present to supervise the donning and doffing process and ensure it is performed correctly
- Healthcare organisations must apply both standard and transmission-based precautions as they are applied individually
- Workers must have a thorough understanding of contact, droplet and airborne precautions
- Strict hand hygiene must be performed.
(CEC 2020; WHO 2019; ACSQHC 2019)
How to Don PPE
- Perform hand hygiene.
- Put on your gown.
- Fully cover your torso from your neck to your knees and your arms to the end of your wrists, then tie at the back.
- The gown should be large enough to allow unrestricted movement without gaping.
- Fasten at the back of the neck and waist.
- Put on your mask or particulate filter respirator.
- Secure the ties or elastic bands at the middle of the head and neck.
- Fit the flexible band to your nose bridge.
- Fit your mask snug to your face and below your chin.
- Fit-check your respirator according to manufacturer instructions.
- Put on your protective eyewear or face shield by placing it over eyes/face and adjusting to fit.
- Perform hand hygiene.
- Put on your gloves, extending them to cover the wrist of your gown.
(ACSQHC 2024; SA Health 2024; CEC 2020)
Remember to always refer to the World Health Organisation’s ‘5 Moments for Hand Hygiene’.

How to Doff PPE
Following a correct doffing procedure is especially crucial in the control and prevention of infection. It is the most important step in preventing infection transmission (CEC 2020).
Doffing should be performed in a way that protects your clothing, skin and mucous membranes from contamination (VIC DoH 2022).
Remember that all PPE is contaminated after use. Perform hand hygiene immediately after each step of doffing.
Begin doffing at the patient’s doorway (if standard, contact or droplet precautions are in place) or in the anteroom (if airborne precautions are in place). Eye protection and mask/respirator must be removed after exiting the patient’s room (SA Health 2024; ACSQHC 2024).
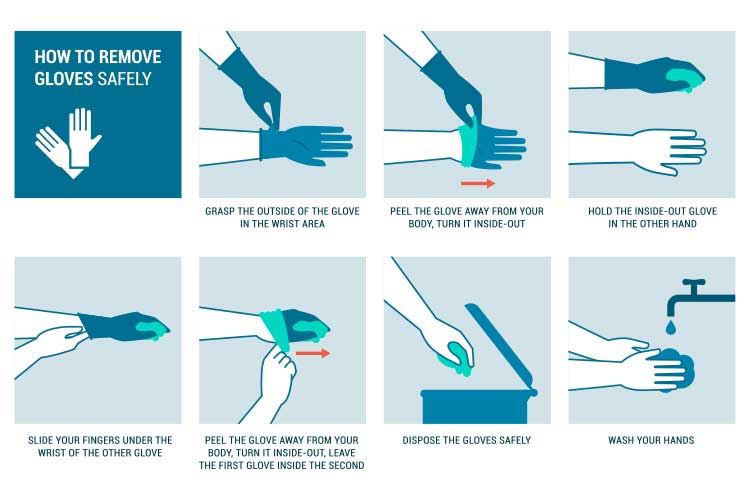
- Remove your gloves.
- Using one hand, grasp the palm of the other hand and peel off the first glove.
- Hold the dirty glove in the hand that is still gloved.
- Slide fingers of the ungloved hand under the remaining glove at the wrist and peel it off over the first glove.
- Discard gloves in a waste container.
- Perform hand hygiene.
- Remove your gown.
- Unfasten the ties, ensuring the sleeves don’t make contact with your body.
- Pull the gown away from your neck and shoulders, touching the inside only.
- Turn the gown inside out.
- Fold or roll the gown into a bundle and discard in the waste container.
- Perform hand hygiene.
- Exit the patient’s room.
- Remove your goggles/face shield.
- Remove from the back of the head by lifting the headband or ear pieces.
- If reusable, place it in the designated reprocessing receptacle. If not, discard in an appropriate waste container.
- Perform hand hygiene.
- Remove your mask/respirator.
- Grasp the bottom ties/elastics, then the top ones, and remove without touching the front of the mask.
- Discard in the waste container.
- Immediately perform hand hygiene.
(ACSQHC 2024; SA Health 2024; CEC 2020)
Remember that PPE must be disposed of after use unless it is marked as reusable. Reusable PPE must be reprocessed before being used again (CEC 2020).
Other Considerations
- If PPE is not worn correctly, there is a high risk of contamination. Always follow hospital protocol and notify your supervisor if necessary.
- If goggles and masks are worn for too long, they may cause pressure injuries to the face. Ensure you protect bony prominences and/or change PPE frequently if possible.
- Always remember to engage with the patient, as it can be quite confronting for them not to see the healthcare worker’s face.
- Take regular breaks if you can.
Conclusion
Correct PPE use is crucial to infection control and prevention. You must always ensure that correct procedures for donning and doffing are followed, and that staff are well-trained and competent.
Always refer to your organisation’s policies and procedures.
Test Your Knowledge
Question 1 of 3
Why is it important to perform hand hygiene after each step during the doffing process?
Topics
Further your knowledge
 Free
Free Free
Free Free
Free
References
- Australian Commission on Safety and Quality in Health Care 2024, Sequence for Putting on and Removing Personal Protective Equipment (PPE), Australian Government, viewed 30 April 2025, https://www.safetyandquality.gov.au/sites/default/files/2024-06/sequence-putting-and-removing-personal-protective-equipment-ppe.pdf
- Clinical Excellence Commission 2020, PPE for Combined Contact, Droplet and Airborne Precautions, online video, 7 April, YouTube, viewed 30 April 2025, https://www.youtube.com/watch?v=tfITL694UAQ
- MedlinePlus 2023, Personal Protective Equipment, U.S. Department of Health and Human Services, viewed 30 April 2025, https://medlineplus.gov/ency/patientinstructions/000447.htm
- SA Health 2024, Sequence for Donning (Putting on) and Doffing (Taking off) Personal Protective Equipment, Government of South Australia, viewed 30 April 2025, https://www.sahealth.sa.gov.au/wps/wcm/connect/759d0d97-e9a4-480d-949a-a8316027e028/20015.18+PPE+Sequencing+A3+Poster_June+2024.pdf?MOD=AJPERES&CACHEID=ROOTWORKSPACE-759d0d97-e9a4-480d-949a-a8316027e028-p182-Ld
- Safe Work NSW 2020, Personal Protective Equipment (PPE), New South Wales Government, viewed 30 April 2025, https://www.safework.nsw.gov.au/safety-starts-here/physical-safety-at-work-the-basics/personal-protective-equipment-ppe
- Victoria Department of Health 2022, Donning and Doffing PPE, Victoria State Government, viewed 30 April 2025, https://www.health.vic.gov.au/media/19448
 New
New