In order to accurately and correctly assess a patient using 12-lead monitoring, it is necessary to understand how ECG works, know how to prepare the patient and be able to follow the standardised system for electrodes and their placements.
What is an ECG?
An electrocardiogram (ECG) is a non-invasive method of monitoring the electrophysiology of the heart (Mayo Clinic 2024).
An ECG machine records changes in electrical activity by drawing on moving paper known as an electrocardiograph. The paper moves at a speed of 25 mm per second, and the ECG machine plots time on the x-axis and voltage on the y-axis. On the electrocardiograph, one second is represented by five large squares. These large squares are broken into five smaller squares, representing 0.04 seconds each. When the ECG machine plots the patient’s electrical activity, an increase of one mVolt in voltage moves the stylus by 1 cm (Sattar & Chhabra 2023).
While ECG is commonly used across a variety of medical settings, it plays a particularly important role in the haemodynamic assessment of patients who are cared for in the critical care environment, such as the intensive care unit (Khan 2020).
All ICU patients generally require continuous ECG monitoring if clinically unstable. Continuous ECG monitoring can improve the detection of clinical deterioration (Khan 2020; Moss et al. 2017).
How Does an ECG Work?
An ECG involves the placement of electrodes onto the patient’s torso and/or limbs. The electrodes are connected to an electrocardiograph, which displays a pictorial representation of the patient’s cardiac activity (Better Health Channel 2023).
The waves detected and visually displayed through ECG illustrate the sequence of depolarisation (positive current) and repolarisation (negative current) generated by action potentials (electrical impulses) of the atria and ventricles in the heart (Klabunde 2023a).
What is 12-Lead ECG?
ECG measures the electrical activity of the heart from several leads (viewpoints) in order to construct a picture of the patient's cardiac function using voltage on the vertical axis against time on the horizontal axis (Cables and Sensors 2024).
Each lead has its own code name and represents the voltage difference between two electrodes. There are two types of leads:
| Lead type | Leads included | How they work |
| Bipolar leads (i.e. standard limb leads) | I, II, III | Measure the voltage difference between one positive electrode and one negative electrode. |
| Unipolar leads (i.e. augmented leads and chest leads) |
|
Have a single positive electrode and use a combination of the other electrodes as a composite negative electrode. |
(Cables and Sensors 2024; Klabunde 2023b)
Commonly used lead systems include:
- 3-lead monitoring, which uses 3 electrodes on the torso
- 5-lead monitoring, which uses 5 electrodes on the torso
- 12-lead monitoring, which uses 10 electrodes on the torso and limbs.
(Cadogan 2022)
12-lead monitoring is generally considered the standard form of ECG and provides the most information.
Preparing a Patient for a 12-Lead ECG
As with all procedures, you must obtain informed consent from the patient by explaining the purpose of the procedure, describing the procedure itself and obtaining consent to proceed. Maintain good infection control practice by washing your hands prior to patient contact.
Skin preparation is important. If the patient’s skin is dirty, clean with soap and water and then dry. If the skin is oily or the patient has applied any creams or lotions, use an alcohol wipe to clean each electrode placement site.
Some ECG machines may also provide a ‘rough patch’ either separately or on the electrodes, which can be used to rub on the skin to increase electrode adherence. Care should be taken not to cause abrasions.
Patients with chest hair should have hair at the electrode placement sites removed with a hair clipper (Cables and Sensors 2024).
Where possible, place the patient in a supine or semi-recumbent position with their legs and arms uncrossed (QAS 2024). If this is not possible or is uncomfortable for the patient, it is acceptable to record the ECG in another position.
The patient must be completely relaxed. Ensure the environment is comfortably warm to prevent shivering (Sattar & Chhabra 2023). This will prevent muscular tension or movements from producing artefacts on the ECG recording. Ensure the patient’s privacy and dignity, e.g. by closing the room door or drawing around the curtains.
12-Lead Placement
Correct placement of electrodes is crucial.
The placement of electrodes for ECG monitoring is standardised to ensure that the information gathered is accurate and can be compared with records from other occasions. To ensure accurate results, the patient must also be correctly prepared both physically and psychologically (ADInstruments 2025).
Poor electrode placement can result in mistaken interpretation, which can lead to possible misdiagnosis, patient mismanagement and inappropriate procedures (Handzel 2023).
The ‘Angle of Louis’ Method can be used to identify the correct landmarks for ECG electrode placement (Sattar & Chhabra 2023).
ECG electrodes are colour-coded, and each is identified by a specific code that refers to its intended placement. There are two coding systems currently in use:
- American Heart Association (AHA) system
- International Electrotechnical Commission (IEC) system.
Both systems are described in the table below.
| Code (AHA) | Code (IEC) | Location | Colour (AHA) | Colour (IEC) |
|---|---|---|---|---|
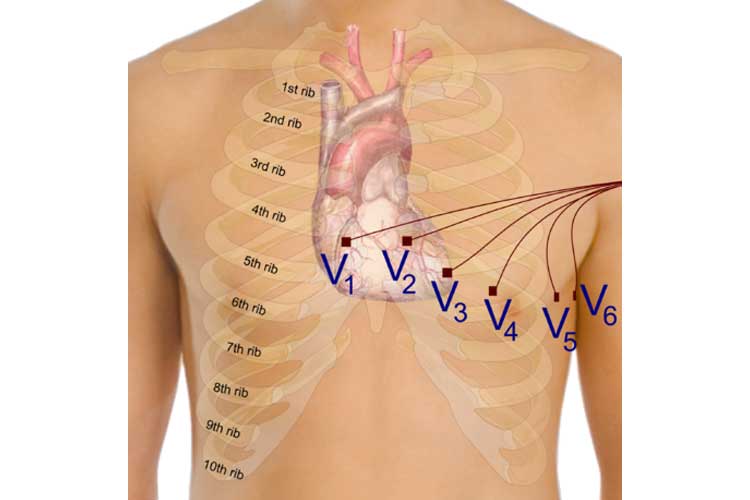
| V1 | C1 | Fourth intercostal space at the right sternal border | Brown/red | White/red |
| V2 | C2 | Fourth intercostal space at the left sternal border | Brown/yellow | White/yellow |
| V3 | C3 | Halfway between leads V2 and V4 | Brown/green | White/green |
| V4 | C4 | Fifth intercostal space in the midclavicular line | Brown/blue | White/brown |
| V5 | C5 | Left anterior axillary line on the same horizontal plane as V4 | Brown/orange | White/black |
| V6 | C6 | Left midaxillary line on the same horizontal plane as V4 and V5 | Brown/purple | White/purple |
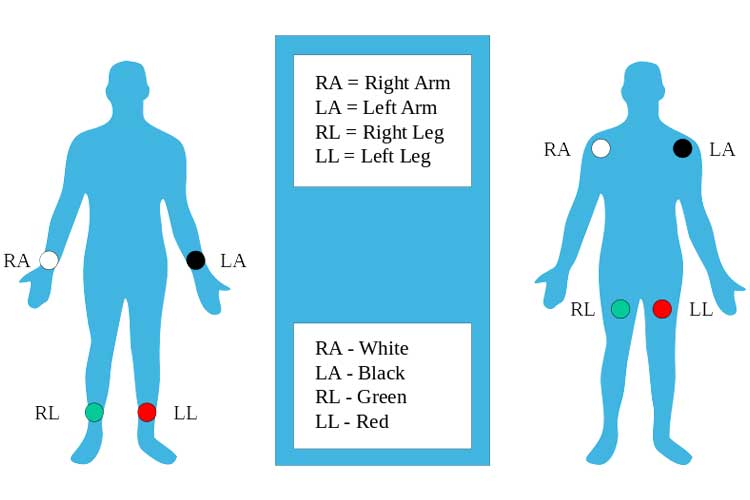
| RA | R | Right arm (inner wrist) | White | Red |
| LA | L | Left arm (inner wrist) | Black | Yellow |
| RL | N | Right leg (inner ankle) | Green | Black |
| LL | F | Left leg (inner ankle) | Red | Green |
(ADInstruments 2025; Cables and Sensors 2024; Cadogan 2022)
Precordial Lead Placement
Note: The following guide uses the AHA system.
In order to find these correctly, the ‘Angle of Louis’ Method can be used:
- To locate the space for V1; locate the sternal notch (Angle of Louis) at the second rib and feel down the sternal border until the fourth intercostal space is found. V1 is placed to the right of the sternal border, and V2 is placed at the left of the sternal border.
- Next, V4 should be placed before V3. V4 should be placed in the fifth intercostal space in the midclavicular line (as if drawing a line downwards from the centre of the patient’s clavicle).
- V3 is placed directly between V2 and V4.
- V5 is placed directly between V4 and V6.
- V6 is placed over the fifth intercostal space at the mid-axillary line (as if drawing a line down from the armpit).
- V4-V6 should line up horizontally along the fifth intercostal space.
(Sattar & Chhabra 2023)
Limb Lead Placement Diagram
Other Considerations
In female patients, the V4, V5 and V6 leads are recommended to be placed underneath the left breast where the breast tissue meets the chest (GE HealthCare 2022).
It is also customary practice to record any necessary alterations in lead placement, such as when lead placement is changed from the standardised location due to patient position, injury, etc.
End of Procedure
Ensure that the patient’s privacy and dignity are maintained. The chest should not be left exposed and should be covered back up with blankets, or the patient can re-dress as necessary.
The ECG electrodes should be removed if the patient is not likely to require further or serial ECGs, but otherwise can be left in place for up to 24 hours before needing to be replaced (Danlee Medical Products 2024).
If you are not interpreting the ECG, follow local policy and use clinical judgement to arrange for interpretation. Local policies often also require the initials of the person taking the ECG to be recorded.
Test Your Knowledge
Question 1 of 3
Why is it important to ensure a warm environment during ECG recording?
Topics
Further your knowledge
 Free
Free Free
Free
References
- ADInstruments 2025, ‘Correct 12 Lead ECG Placement for Researchers – A Simple Guide’, ADInstruments Blog, 5 March, viewed 29 April 2025, https://www.adinstruments.com/blog/correctly-place-electrodes-12-lead-ecg
- Better Health Channel 2023, ECG Test, Victoria State Government, viewed 29 April 2025, https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/ecg-test
- Cables and Sensors 2024, 12-Lead ECG Placement Guide with Illustrations, Cables and Sensors, viewed 29 April 2025, https://www.cablesandsensors.com/pages/12-lead-ecg-placement-guide-with-illustrations
- Cadogan, M 2022, ECG Lead Positioning, Life in the Fastlane, viewed 29 April 2025, https://litfl.com/ecg-lead-positioning/
- Danlee Medical Products 2024, How to Use ECG Electrodes, Danlee Medical Products, viewed 18 June 2025, https://www.danleemedical.com/blog/how-to-use-ecg-electrodes/
- GE HealthCare 2022, ‘Best Practices for ECG Lead Placement on Women’, Insights, 17 February, viewed 18 June 2025, https://www.gehealthcare.com/insights/article/best-practices-for-ecg-lead-placement-on-women
- Handzel, S 2023, ‘ECG Lead Misplacement: Looking at Common Issues’, Insights, 18 August, viewed 29 April 2025, https://www.gehealthcare.com/insights/article/ecg-lead-misplacement-looking-at-common-issues
- Khan, F 2020, ‘ECG in the ICU Patient’, in WJ Brady et al. (eds.), Electrocardiogram in Clinical Medicine, John Wiley & Sons, UK, viewed 29 April 2025, https://onlinelibrary.wiley.com/doi/epdf/10.1002/9781118754511.ch34?saml_referrer
- Klabunde, RE 2023a, Electrocardiogram (EKG, ECG), Cardiovascular Physiology Concepts, viewed 29 April 2025, https://cvphysiology.com/Arrhythmias/A009
- Klabunde, RE 2023b, Electrocardiogram Leads, Cardiovascular Physiology Concepts, viewed 29 April 2025, https://www.cvphysiology.com/Arrhythmias/A013
- Moss, TJ, Clark, MT, Calland, JF et al. 2017, ‘Cardiorespiratory Dynamics Measured from Continuous ECG Monitoring Improves Detection of Deterioration in Acute Care Patients: A Retrospective Cohort Study’, Plos One, viewed 19 April 2025, https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0181448
- Mayo Clinic 2024, Electrocardiogram (ECG or EKG), Mayo Clinic, viewed 29 April 2025, https://www.mayoclinic.org/tests-procedures/ekg/about/pac-20384983
- Queensland Ambulance Service 2024, Clinical Practice Procedures: Cardiac/12-Lead ECG Acquisition, Queensland Government, viewed 17 June 2025, https://www.ambulance.qld.gov.au/clinical/cpm/procedures
- Sattar, Y & Chhabra, L 2023, ‘Electrocardiogram’, StatPearls, viewed 29 April 2025, https://www.ncbi.nlm.nih.gov/books/NBK549803/
 New
New