What is Guillain-Barré Syndrome (GBS)?
Let’s face it: you’re probably thinking, ‘How do I say it?’
Guillain-Barré is pronounced ‘ghee-yan bah-ray’, named after the three French neurologists who first described the condition (Brain Foundation 2021).
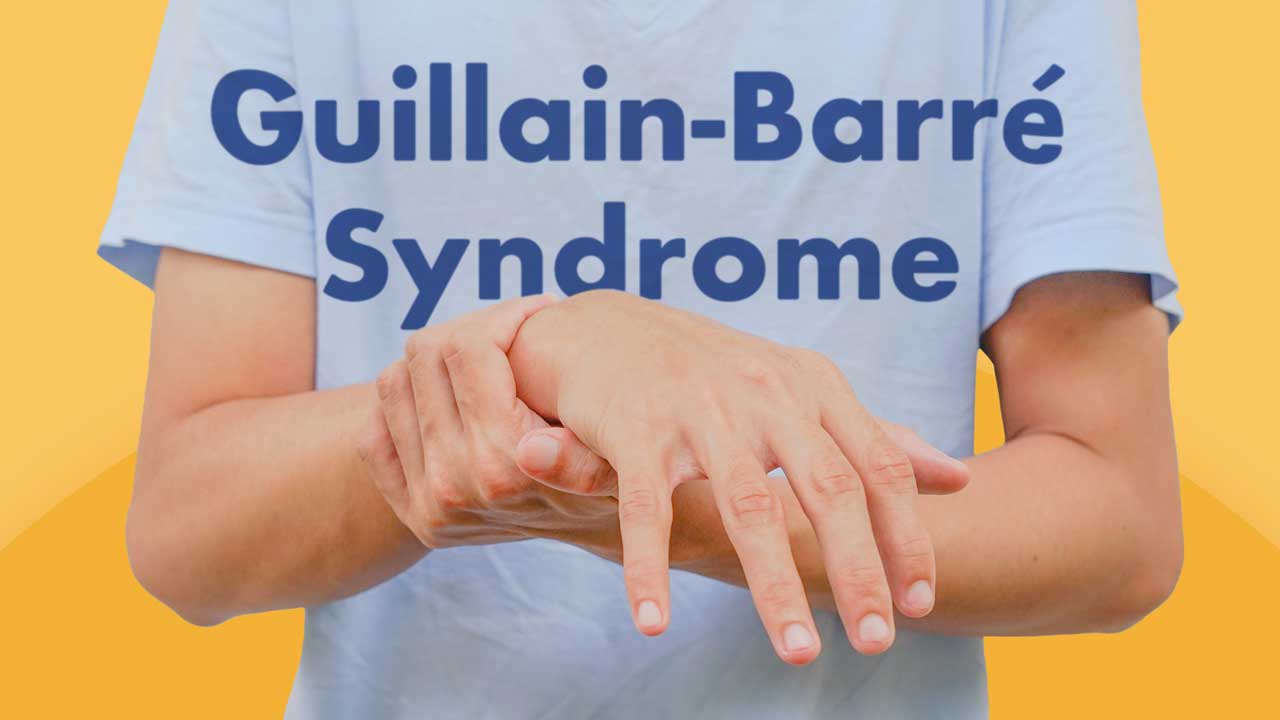
GBS is an autoimmune disease in which the peripheral nerves and nerve roots are damaged by the immune system’s antibodies and lymphocytes (Brain Foundation 2021).
The myelin (nerve insulation) and sometimes the axon (the inner covered part of the nerve) of the nerves are damaged, causing delays and changes to the signals being transmitted between the nerves and the brain (Better Health Channel 2014).
Patients will often present with progressive bilateral and symmetrical weakness and paralysis of the lower limbs, as well as disturbing sensory sensations (Better Health Channel 2014).
These abnormal sensations are known as paraesthesia. Patients may experience feelings such as tingling, formications or pain (NINDS 2023).
Symptoms usually begin in the feet or legs, gradually spreading up the body as the condition progresses. Less commonly, they begin in the arms and progresses downward (Better Health Channel 2014).
Although the exact cause of GBS is unknown, it usually seems to be triggered by a viral or bacterial infection and is not considered contagious (Better Health Channel 2014).
Symptoms of Guillain-Barré Syndrome
Patients may experience:
- Muscle weakness and bilateral paralysis
- Jerky, uncoordinated movements
- Numbness
- Muscle aches, pains or cramps
- Disturbed sensations such as vibrations, buzzing or pins and needles
- Blurred vision
- Dizziness
- Breathing difficulties.
(Better Health Channel 2014)
Possible complications of GBS include deep vein thrombosis, respiratory failure, pressure injuries and pneumonia, among others (Better Health Channel 2014; Mayo Clinic 2022).
Generally, symptoms progress over days or weeks before reaching a plateau. The time in which a patient will reach this plateau varies but it is usually up to four weeks after the initial onset of symptoms (Better Health Channel 2014; Nguyen & Taylor 2023).
GBS can range from mild to severe. In the most severe cases, the nerves controlling respiratory function and the autonomic nervous system may be affected and the individual may require life support. Once the autonomic nervous system is affected, the individual may experience changes to their blood pressure, heart rate, vision, kidney function and temperature regulation (Better Health Channel 2014; NINDS 2023).
Note that GBS is relatively rare, with roughly 2 to 8 people affected out of every 100,000. It seems to be more common among those aged 30 to 50, but can affect people of any age (Garvan Institute 2020).
Causes of Guillain-Barré Syndrome
The exact cause of GBS remains unknown (Better Health Channel 2014). However, in up to 70% of cases, the onset of symptoms is preceded one to six weeks earlier by an infection (Nguyen & Taylor 2023).
GBS is most often linked to gastrointestinal and respiratory infections, particularly Campylobacter jejuni (Andary 2022).
Other infections associated with GBS include cytomegalovirus (CMV), COVID-19, Epstein-Barr virus (EBV), varicella-zoster virus, human immunodeficiency virus (HIV) and possibly Zika virus (Andary 2022).
Events that may trigger GBS include pregnancy, surgical procedures, insect bites, Bell’s palsy, and some COVID-19 vaccines (Better Health Channel 2014; Andary 2022).
Diagnosing Guillain-Barré Syndrome
The difficulty in diagnosing GBS is mainly due to the range of symptoms the individual presents with, as they may appear vague and unrelated to each other. Diagnosis often requires several tests including physical examination, muscle strength and activity tests, reflex tests, nerve conduction tests and spinal taps to check for increased protein in the cerebral spinal fluid (Better Health 2014).
How is Guillain Barré Syndrome Treated?
Due to the unpredictability of GBS, most patients are admitted to hospital for monitoring. If any complications occur that might affect vital functions, treatment can then be initiated immediately (Better Health Channel 2014).
There is no cure for GBS, but there are some treatment options. Intravenous immunoglobulin (IVIG) infusions can be administered over a period of five days to help lessen the immune attack on the nervous system. However, it is not completely known how or why this works (Nguyen & Taylor 2023).
Plasmapheresis can also be undertaken. This involves taking blood from the patient, removing the immune cells and then returning the remaining red blood cells to the body (Better Health Channel 2014).
Both options are effective in reducing the severity of GBS and assisting in recovery (Nguyen & Taylor 2023).
Recovery and Rehabilitation
Recovery from GBS varies. About 95% of patients survive, with 80% ambulating independently after six months and 60% fully recovering their motor strength within one year. Less than 20% of patients will live with disability as a result of GBS (Nguyen & Taylor 2023; Andary 2022).
Generally, recovery is more likely among patients whose symptoms begin to ease earlier (Better Health Channel 2014).
As with any neurological condition, assessment of the patient upon entry to rehabilitation is essential. This assessment should include the clinical history of the patient, initial presentation and any other medical conditions as well as other presenting symptoms such as paralysis, sensation disturbances, fatigue, spasticity and muscle tone (Mauk 2012).
Assessment is important in order to plan and implement a successful rehabilitation program for the patient. A rehabilitation program will often include extensive therapy from an interprofessional team (Better Health Channel 2014).

Nursing Care of Guillain-Barré Syndrome
The role of a nurse during rehabilitation is complementary to the rest of the interprofessional team and involves providing critical education to the patient and family, as well as support and reassurance during recovery.
This education can encompass a variety of areas and will differ depending on the specific individual and their lifestyle. Often, the education will be provided to help ensure adherence to treatment recommendations made by the interprofessional team (Mauk 2012). Education may involve strategies for mobilising and eating safely or medication management for when the patient is discharged home.
As mentioned above, recovery from GBS varies. 30% of patients will still have some residual weakness three years following the event, with 3% suffering further relapses of muscle weakness and tingling for many years after the initial illness (NINDS 2023).
Recovery may also be hampered by the emotional and psychological difficulties associated with GBS, especially for those with residual and permanent disability following the illness (NINDS 2023).
The nursing care of patients with GBS should be varied and holistic, taking into account where the patient is at in their recovery.
Key points of nursing care include:
- Watching for blood clots and DVT
- Monitoring vital signs closely
- Minimising falls risk, taking weakness and paralysis into consideration
- Providing pain management appropriate to the individual - evidently, there will be a need to consider the types of analgesics used and their potential side effects
- Helping the client control their body temperature
- Completing regular, thorough observations and assessments (including respiratory assessments)
- Referring to other health professionals in the interprofessional team (e.g. physiotherapists to improve mobility)
- Educating patients, family members and carers.
Test Your Knowledge
Question 1 of 3
How long after onset do the symptoms of Guillain-Barré syndrome generally tend to plateau?
Topics
References
- Andary, MT 2022, Guillain-Barre Syndrome, Medscape, viewed 12 September 2023, https://emedicine.medscape.com/article/315632-overview#a4
- Better Health Channel 2014, Guillain-Barré Syndrome, Victoria State Government, viewed 12 September 2023, https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/guillain-barre-syndrome
- Brain Foundation 2021, Guillain-Barre Syndrome, Brain Foundation, viewed 12 September 2023, https://brainfoundation.org.au/disorders/guillain-barre-syndrome/
- Garvan Institute 2020, Guillain-Barré Syndrome, Garvan Institute, viewed 12 September 2023, https://www.garvan.org.au/research/diseases/guillain-barre-syndrome
- Mauk, KL 2012, Rehabilitation Nursing: A Contemporary Approach to Practice, Jones & Bartlett Learning, Sudbury.
- Mayo Clinic 2022, Guillain-Barre Syndrome, Mayo Clinic, viewed 12 September 2023, https://www.mayoclinic.org/diseases-conditions/guillain-barre-syndrome/symptoms-causes/syc-20362793
- National Institute of Neurological Disorders and Stroke 2023, Guillain-Barré Syndrome, U.S. Department of Health and Human Services, viewed 12 September 2023, https://www.ninds.nih.gov/health-information/disorders/guillain-barre-syndrome
- Nguyen, TP & Taylor, RS 2023, ‘Guillain-Barre Syndrome’, StatPearls, viewed 12 September 2023, https://www.ncbi.nlm.nih.gov/books/NBK532254/
 New
New