For patients who do not have the capacity to communicate, pain can be overlooked, causing significant but unnecessary discomfort and distress.
Defining Pain
Pain is complex, subjective and varying. The International Association for the Study of Pain (2022) defines pain as ‘An unpleasant sensory and emotional experience associated with, or resembling that associated with, actual or potential tissue damage’.
Pain can range from mild to severe, affecting a localised area or several parts of the body. It is a highly personal experience that varies in intensity depending on the individual, even if caused by the same stimulus (Shiel 2018).
In addition to causing physical discomfort, pain can also have implications on an individual’s emotional or mental wellbeing as well as their daily life (Healthdirect 2021).
Pain can be acute or chronic:
- Acute pain is usually temporary and sudden, with a clearly defined trigger. It eventually resolves once the underlying cause has been addressed.
- Chronic pain is persistent, often lasting for weeks, months or years. It may be triggered by an underlying condition, be a condition in its own right, or have no clear cause.
(Shiel 2018; Healthdirect 2021)
Pain Statistics
Pain is prevalent, especially among older adults and people living with medical conditions.
- One in five Australians over 45 are living with chronic pain.
- One in three adults over 65 are living with chronic pain.
- Up to 80% of aged care residents are living with chronic pain.
(AIHW 2020; Painaustralia 2021)
People living with the following conditions have reported experiencing chronic pain:
- Alzheimer’s disease and other types of dementia
- Effects of stroke
- Chronic lung disease
- Cancers
- Asthma heart disease
- Diabetes
- Osteoporosis
- Mental illness
- Hypertension
- Arthritis
- Other long-term conditions or injuries.
(AIHW 2020)
Communicating Pain
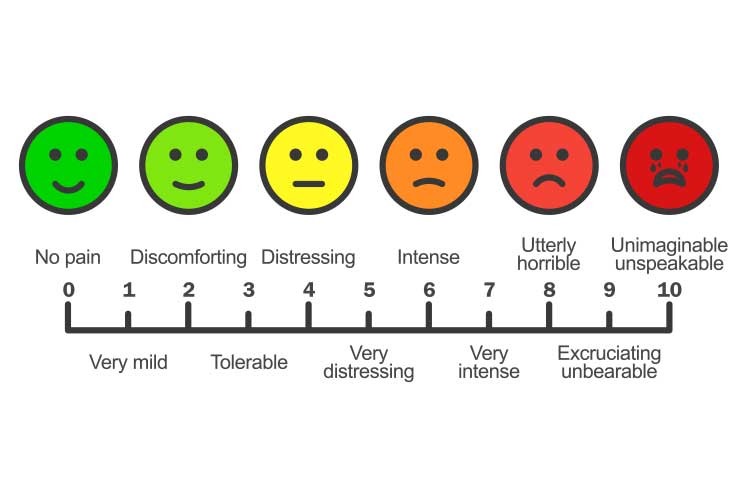
The highly subjective nature of pain means that the best person to measure and describe the pain is the individual experiencing it. Patient self-reports are the most reliable gauge (Shiel 2018).
However, some patients may not have the capacity to self-report their pain. The process of discussing and assessing pain is a complicated social transaction between patient and healthcare professional, and if the patient is unable to communicate their pain, it becomes difficult to appropriately respond to and treat their discomfort (Boekel et al. 2017).
A study found that 1 in 10 patients self-report a low level of pain even if the pain is considered unacceptable. This poses serious questions and concerns about those who cannot communicate their pain at all (Boekel et al. 2017).
In addition to being a physically uncomfortable experience, untreated pain may also:
- Cause unnecessary suffering
- Worsen cognitive impairments
- Cause the patient to become agitated
- Impair the patient’s quality of life
- Delay recovery
- Interfere with daily life
- Cause psychological distress
- Cause breathing difficulties leading to respiratory deterioration
- Cause immobilisation
- Impair physical function
- Increase the risk of falls.
(Booker & Haedtke 2016; McGuire et al. 2016; Gan 2017)
When a patient is unable to verbally express their discomfort, you should use assessment tools and observe for any pain behaviours. This is imperative to ensure all patients are comfortable and nobody is unknowingly suffering (Booker & Haedtke 2016).
Who Might be Unable to Communicate Pain?
- Post-anaesthetic patients
- Patients with cognitive impairment (e.g. dementia)
- Patients receiving palliative care
- Patients receiving end-of-life care
- Deaf or hard of hearing patients
- Intubated patients
- Sedated or unresponsive patients
- Patients with aphagia
- Neurologically compromised patients
- Patients who have fears, beliefs and misconceptions about their pain
- Patients who have specific cultural needs
- Patients who have difficulty with literacy and numeracy skills.
(Booker & Haedtke 2016; McGuire et al. 2016; Marie Curie 2022; Health.vic 2021)

Non-Verbal Pain Assessment Tools
There many tools that may be used to assess non-verbal patients. The following are some widely-used examples - please note that this is not a comprehensive list of every tool available.
- Abbey Pain Scale
- Pain Assessment Checklist for Seniors With Limited Ability to Communicate (PACSLAC)
- The Pain Assessment in Advanced Dementia Scale (PAINAID)
(Health.vic 2021)
Note: Always refer to your facility’s policies and procedures when selecting and using pain assessment tools.
Non-Verbal Clinical Signs and Symptoms of Pain
The following behaviours may suggest the presence of pain in adults who are unable to communicate:
| Facial expressions | Rapid blinking, fear, brow lowering, clenched teeth, narrowing or closure of eyes, upper lip raising, nose wrinkling. |
| Verbalisations | Screaming, swearing, crying, moaning, sighing, making fewer sounds than is typical. |
| Body movements | Gaiting, limping, rubbing a body area, muscle rigidity, decreased movement, guarding, pacing, rocking, fidgeting, repetitive movements, reluctance to move, decreased range of movement. |
| Interpersonal interactions | Resisting care, aggression, withdrawal, isolation. |
| Mood and mental state | Delirium, depressive state, agitation, anxiety, irritability, crying, impaired executive function, declining cognition, worsening of cognitive impairment, confusion, restlessness. |
| Activity | Wandering, sleep disturbances, increased sleep, social disengagement, change of routine, staying in bed, low appetite. |
| Function | Decreased ability to function in daily life, falls. |
| Autonomic signs | Pallor, altered breathing, change in vital signs, sweating. |
(Adapted from Booker & Haedtke 2016; Dementia Australia 2015)
Note: These signs may be unrelated to pain and caused by another condition. Some patients experiencing pain may display few or none of these signs (Dementia Australia 2015).

Challenges Faced by Healthcare Professionals
A study identified the following challenges experienced by nurses that may inhibit the assessment of pain in non-verbal patients:
- Pain assessment of non-verbal patients not being routine
- Lack of relevant policies and procedures
- Inadequate discussions about pain between nurses and physicians
- Lack of assessment tools in the nursing flowchart
- Inadequate nurse-to-patient ratios
- Limited or no experience in using non-verbal assessment scales
- The belief that sedated patients do not need additional pain relief
- Lack of understanding regarding pain in unconscious patients
- The belief that non-verbal assessment tools are ineffective
- Unfamiliarity with non-verbal pain scales
- Lack of training in non-verbal pain scales.
(Deldar et al. 2018)
Identifying and remedying these barriers to effective pain assessment will help improve the quality of care delivered to non-verbal patients (Deldar et al. 2018).
Conclusion
Sourcing and using appropriate assessment tools for patients who are unable to communicate their pain is crucial. Poorly-managed pain can lead to other health complications and unnecessary discomfort and distress.
Thorough assessments should be performed to identify and manage pain experienced by non-verbal patients - being unable to verbalise their discomfort means they are relying on healthcare professionals to ensure they are comfortable and not quietly suffering.
Test Your Knowledge
Question 1 of 3
True or false: Different people may respond to the same pain stimulus differently.
Topics
References
- Australian Institute of Health and Welfare 2020, Chronic Pain in Australia, Australian Government, viewed 6 June 2023, https://www.aihw.gov.au/getmedia/10434b6f-2147-46ab-b654-a90f05592d35/aihw-phe-267.pdf.aspx?inline=true
- Boekel et al. 2017, ‘Moving Beyond Pain Scores: Multidimensional Pain Assessment is Essential for Adequate Pain Management After Surgery’, PLoS One, vol. 12 no. 5, viewed 5 June 2023, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5425226/
- Booker, S Q & Haedtke, C 2016, ‘Assessing Pain in Nonverbal Older Adults’, Nursing, vol. 46 no. 5, viewed 6 June 2023, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4991889/
- Deldar, K, Froutan, R & Ebadi, A 2018, ‘Challenges Faced by Nurses in Using Pain Assessment Scale in Patients Unable to Communicate: Qualitative Study’, BMC Nursing, viewed 6 June 2023, https://bmcnurs.biomedcentral.com/articles/10.1186/s12912-018-0281-3
- Dementia Australia 2015, What are Some Non-Verbal Signs of Pain?, Dementia Australia, viewed 6 June 2023, https://www.dementia.org.au/files/Dementia%20Stroke%20CHD%20Fact%20Sheet%202%20V5.pdf
- Gan, TJ 2017, ‘Poorly Controlled Postoperative Pain: Prevalence, Consequences, and Prevention’, J Pain Res., vol. 10, viewed 6 June 2023, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5626380/
- Healthdirect 2021, Chronic Pain, Australian Government, viewed 6 June 2023, https://www.healthdirect.gov.au/chronic-pain
- Health.vic 2021, Identifying Pain, Victoria State Government, viewed 6 June 2022, https://www.health.vic.gov.au/patient-care/identifying-pain
- International Association for the Study of Pain 2022, Terminology, IASP, viewed 6 June 2023, https://www.iasp-pain.org/resources/terminology/
- Marie Curie 2022, Communication Needs in Palliative Care, Marie Curie, viewed 6 June 2023, https://www.mariecurie.org.uk/professionals/palliative-care-knowledge-zone/individual-needs/communication-needs
- McGuire, DB, Kaiser, KS, Haisfield-Wolfe, ME & Iyamu, F 2016, ‘Pain Assessment in Non-Communicative Adult Palliative Care Patients’, Nurs Clin North Am., viewed 6 June 2023, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4978178/
- Painaustralia 2021, Older People & Those Living With a Disability, Painaustralia, viewed 6 June 2023, https://www.painaustralia.org.au/about-pain/who-it-affects-pages-2021/older-people-those-living-with-a-disability-2021
- Shiel, WC 2018, Pain (Acute and Chronic), MedicineNet, viewed 5 June 2023, https://www.medicinenet.com/pain_acute_and_chronic/views.htm
 New
New 
