Mastitis is a spectrum of painful conditions that affects approximately one in five breastfeeding mothers in the first six months after birth (Mitchell et al. 2022; Liotta 2021).
Characterised by an area of inflamed breast tissue and accompanied by pain and fever, it’s a distressing condition that can negatively impact the ability to breastfeed.
Note: This article has been updated in response to updated guidelines from the Academy of Breastfeeding Medicine.
What Causes Mastitis?
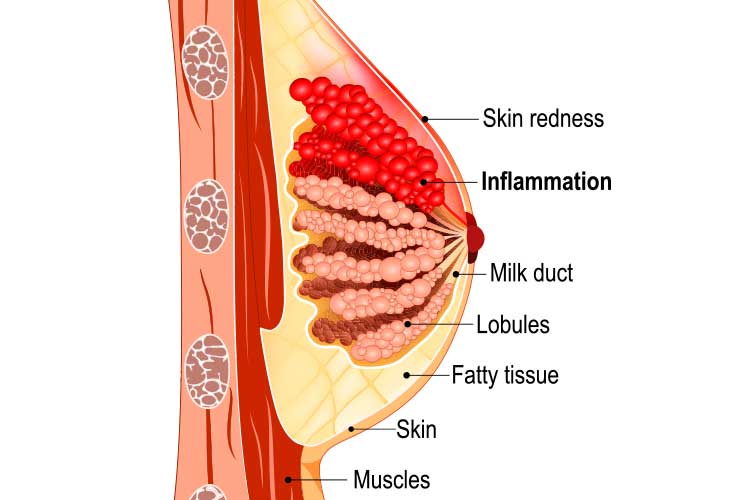
Mastitis is believed to be caused by inflammation of the breast tissue, leading to the narrowing of the milk ducts. This can occur due to hyperlactation (oversupply of breast milk) and/or mammary dysbiosis (disruption of the milk microbiome due to factors such as genetics and the use of antibiotics and probiotics) (Cook 2023; Minnesota WIC Program 2023; Mitchell et al. 2022).
In cases of infective mastitis, the bacteria responsible is usually Staphylococcus aureus. Other causative bacteria include beta-haemolytic Streptococcus, Escherichia coli and methicillin-resistant S. aureus (The Women’s 2020).
Signs and Symptoms of Mastitis
Mastitis should be suspected if a patient is experiencing:
- A hot and painful breast
- Flu-like symptoms, including fever, chills or increased heart rate
- A tender, red, swollen and/or hard area of the breast. The skin of the affected area might appear shiny or have red streaks.
(ABS 2023)
Treating Mastitis
Treatment for mastitis should start at the first signs of the condition (ABS 2023).
Management should include:
- Maintaining a normal breastfeeding schedule
- Ensuring optimal positioning and attachment during breastfeeding
- Applying a cold pack between breastfeeds to relieve pain and inflammation
- Wearing a supportive and comfortable bra
- Starting each feed on alternate breasts
- Expressing the breast if it still feels full after a feed
- Ensuring rest, adequate hydration and nutrition.
(ABS 2023; Minnesota WIC Program 2023)
Pharmacological Treatments
Paracetamol and ibuprofen are safe to take while breastfeeding and may help to alleviate pain (note, however, that aspirin is not safe to take while breastfeeding) (Pregnancy, Birth and Baby 2020).
Antibiotics should only be prescribed for bacterial mastitis; the use of antibiotics for inflammatory mastitis can disrupt the breast microbiome and result in bacterial mastitis (Mitchell et al. 2022).
Antibiotics are generally safe for breastfed infants; however, they should be monitored for any systemic issues during the antibiotic regimen (The Women’s 2020).
If the patient is severely unwell or is showing signs of sepsis, they will require antibiotics administered intravenously (The Women’s 2020).
Important Observations
Supporting the breastfeeding mother, or checking breast health if the mother chooses to bottle feed, is a core midwifery skill. However, when mastitis is suspected, the following observations become particularly important:
- Assessing vital signs and monitoring for signs of systemic infection
- Assessing breasts and noting the presence of any swelling, erythema or tenderness
- Noting skin quality and presence of cracked nipples that may increase the risk of infection
- Monitoring for signs of potential abscess development
- Observing the infant’s position and latch whilst feeding
- Checking the infant to exclude any anatomical reason for poor latching.
Complications of Mastitis
If not appropriately treated, mastitis can develop into a breast abscess (collection of pus in the breast).
Breastfeeding with Mastitis

While breastfeeding with mastitis can be an uncomfortable and painful experience, it’s important to maintain a normal breastfeeding routine (ABS 2023).
Make sure the infant is positioned and attached optimally, and start each feed on alternate breasts (ABS 2023).
Milk from the affected breast is safe for the infant to drink, although it may have a saltier taste (ABS 2023).
In some cases, the milk from the affected breast will flow more slowly. In order to help stimulate the let-down reflex, patients can try:
- Loosening or removing their bra
- Choosing a comfortable, relaxing position
- Taking deep, even breaths
- Listening to relaxing music
- Skin-to-skin contact with the infant
- Gently stroking the breast towards the nipple
- Warming the breast with a warm gel pack or cloth only before a feed - heat should be avoided at all other times as it can exacerbate inflammation.
(ABS 2023)
If the breast still feels full following a feed, the patient should express to alleviate discomfort (ABS 2023).
Preventing Mastitis
Prevention is always better than cure, and maternity staff are ideally placed to offer advice to patients to reduce the risk of mastitis occurring.
The most important points being:
- Ensuring the infant is properly positioned and attached during feeds
- Feeding as long and often as the infant wants to
- Promptly addressing sore or damaged nipples
- Waking the infant up for a feed if the breasts feel uncomfortably full
- Expressing if the infant is not feeding well
- If weaning, doing so gradually
- Avoiding expressing extra milk if the infant is feeding well
- Avoiding feeding the infant any other fluids unless directed.
(ABS 2023)
Test Your Knowledge
Question 1 of 3
Approximately how many people does mastitis affect in the first six months after birth?
Topics
References
- Australian Breastfeeding Association 2023, Mastitis, ABS, viewed 26 June 2023, https://www.breastfeeding.asn.au/resources/mastitis
- Cook, H 2023, 'The Common Breast Condition We Have Been Treating Wrong', The Sydney Morning Herald, 17 June, viewed 26 June 2023, https://www.smh.com.au/healthcare/the-common-breast-condition-we-have-been-treating-wrong-20230615-p5dgq0.html
- Liotta, M 2021, ‘Prescribing Antibiotics for Women with Mastitis’, newsGP, 6 May, viewed 9 February 2023, https://www1.racgp.org.au/newsgp/clinical/prescribing-antibiotics-for-mastitis
- Minnesota WIC Program 2023, Mastitis: Updated Guidance- Topic of the Month, Minnesota Department of Health, viewed 26 June 2023, https://www.health.state.mn.us/docs/people/wic/localagency/topicmonth/mastitis.pdf
- Mitchell, KB et al. 2022, 'Academy of Breastfeeding Medicine Clinical Protocol #36: The Mastitis Spectrum, Revised 2022', Breastfeeding Medicine, vol. 17, no. 5, viewed 26 June 2023, https://www.bfmed.org/assets/ABM%20Protocol%20%2336.pdf
- Pregnancy, Birth and Baby 2020, Mastitis, Australian Government, viewed 9 February 2023, https://www.pregnancybirthbaby.org.au/mastitis
- The Women’s 2020, Infant Feeding - Mastitis and Breast Abscess, The Women’s, viewed 9 February 2023, https://thewomens.r.worldssl.net/images/uploads/downloadable-records/clinical-guidelines/infant-feeding-mastitis-and-breast-abscess_280720.pdf
 New
New