What is Neurogenic Bladder?
Neurogenic bladder is the overlying term for a variety of urinary dysfunctions caused by a disease or an injury that has disrupted normal neurological functioning (Shenot 2023).
Depending on the nerve damage experienced by the individual, their bladder may become overactive (spastic) or underactive (flaccid) (Cleveland Clinic 2022).
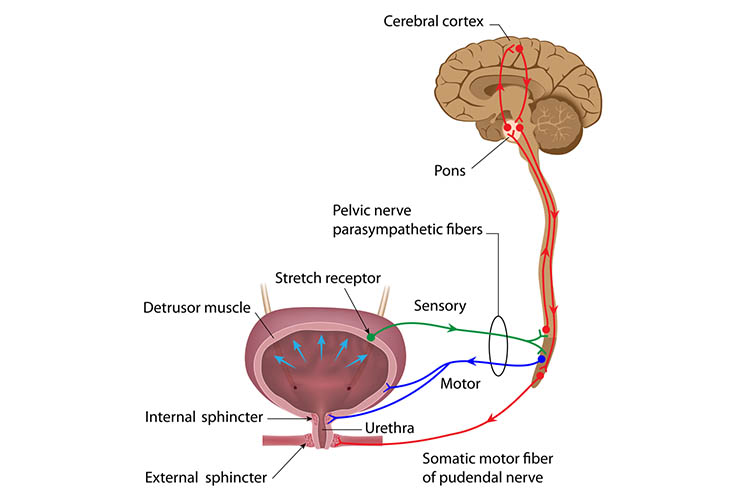
Normal bladder function relies on information traveling through neural pathways from the cerebral cortex through the spinal cord to the bladder to coordinate normal micturition and urinary continence. When this pathway is damaged, it can result in loss of bladder sensation and also the loss of coordination between the urethral sphincter and its muscles (Gill 2022).
Depending on the aetiology and classification of the neurogenic bladder, the individual may experience a variety of symptoms, including:
- Urinary urgency and frequency
- Urinary retention
- Urinary incontinence
- Overflow incontinence
- Urge incontinence
- Erectile dysfunction
- Nocturia
- Spastic paralysis.
(Shenot 2023)
Causes of Neurogenic Bladder
Neurogenic bladder can be caused by any condition that affects the bladder or bladder outlet nerves, including:
- Stroke
- Amyotrophic lateral sclerosis
- Herniated discs
- Parkinson’s disease
- Multiple sclerosis
- Syphilis
- Diabetes
- Infection
- Nerve damage from pelvic surgery
- Trauma or injury to the brain or spinal cord
- Genetic nerve issues
- Heavy metal poisoning
- Birth defects affecting the spinal cord
- Tumors in the brain or spinal cord.
(Shenot 2023; Michigan Medicine 2020)
Classifications of a Neurogenic Bladder
A neurogenic bladder can be classified in many ways, typically depending on the location of the neurologic lesion:
- Supraspinal lesions: These are seen commonly in patients with strokes and brain tumors and often produce an uninhibited bladder. A patient with an uninhibited neurogenic bladder will experience sensation but lack voluntary control, so they may have urgency, frequent bladder contractions and nocturia.
- Spinal cord lesions: These are commonly seen in people with traumatic spinal cord injuries or multiple sclerosis.
- Peripheral nerve lesions: These are commonly seen in people with diabetes, neurosyphilis, herpes zoster or herniated discs or who have undergone pelvic surgery, causing detrusor areflexia (retention).
(Gill 2022)
Investigations and Bladder Assessment
Diagnosis of neurogenic bladder is essential to ensure effective management strategies are implemented. There are a variety of investigations and assessments that need to be completed in order to diagnose a neurogenic bladder and exclude other possible causes. Some of these investigations include:
- Analysis of the urine
- Measurement of residual urine
- Urine flow test
- Filling and voiding cystometry
- Radiological investigations.
(Gill 2022)
Potential Complications of Neurogenic Bladder Dysfunction
In addition to physical complications caused by neurogenic bladder, there may also be negative psychosocial effects, including decreased quality of life and feelings of embarrassment and depression, which can lead to further social isolation. This may be devastating in the case of someone with a progressive neurological condition (Koru Hastanesi 2023).
Potential physical complications of neurogenic bladder include:
- Urinary tract infections
- Bladder damage
- Renal failure
- Urolithiasis (urinary calculi)
- Loss of bladder compliance
- Urethral erosions
- Haematuria
- Renal stones
- Refractory urinary incontinence
- Bladder decompensation
- Malignancy (rarely).
(Leslie et al. 2023)
Management of Neurogenic Bladder

Management of neurogenic bladder needs to be individualized according to factors such as comorbidities, the cause of the dysfunction and the patient’s preferences (Leslie et al. 2023).
The main focus of management is to reduce damage to the upper urinary tract and bladder. The patient needs to be involved in their own bladder management program to ensure it works for them and fits in with their lifestyle. This may mean a combination of bladder training, behavior modification and medications, and as a last resort, surgery may be required (Leslie et al. 2023).
Bladder training is an essential component of neurogenic bladder management. It ensures regular and adequate emptying of the bladder and may be through the means of a voiding schedule or self-catheterization (Leslie et al. 2023).
Intermittent catheterization can be used for patients who have complete or partial urinary retention. Self-administered intermittent catheterization has many benefits over indwelling catheters, including enhanced independence and confidence and fewer long-term complications (Leslie et al. 2023).
Patient education is critical for patients who are self-administering intermittent catheterization, with one of the most frequent complications being urinary tract infections (Leslie et al. 2023).
An indwelling catheter or suprapubic catheter can also be used, but once again, patient education is essential for catheter care on discharge. While this is not the preferred method of long-term bladder management, it may be the most effective and practical solution for people with poor hand function or cognitive impairment, for example (Leslie et al. 2023).
Pharmacological therapies can also be used for bladder management. Surgical interventions are generally implemented as a last resort (Leslie et al. 2023).
Topics
References
- Cleveland Clinic 2022, Neurogenic Bladder, Cleveland Clinic, viewed 6 December 2023, https://my.clevelandclinic.org/health/diseases/15133-neurogenic-bladder
- Gill, BC 2022, Neurogenic Bladder, Medscape, viewed 6 December 2023, https://emedicine.medscape.com/article/453539-overview
- Koru Hastanesi 2023, What Is Neurogenic Bladder?, Koru International Hospital, viewed 6 December 2023, https://www.koruhastanesi.com/what-is-neurogenic-bladder-3705-5
- Leslie, SW, Tadi, P & Tayyeb, M 2023, ‘Neurogenic Bladder and Neurogenic Lower Urinary Tract Dysfunction’, StatPearls, viewed 6 December 2023, https://www.ncbi.nlm.nih.gov/books/NBK560617/#article-25789.s10
- Michigan Medicine 2020, Neurogenic Bladder, University of Michigan, viewed 6 December 2023, https://www.uofmhealth.org/conditions-treatments/adult-urology/neurogenic-bladder
- Shenot, PJ 2023, Neurogenic Bladder, MSD Manual, viewed 6 December 2023, https://www.msdmanuals.com/en-au/professional/genitourinary-disorders/voiding-disorders/neurogenic-bladder
 New
New 
