Pancreatic cancer has an unfortunately high mortality rate due to the lack of obvious symptoms in its early stages. In many cases, by the time it’s diagnosed, the cancer has already advanced significantly.
In fact, the five-year survival rate for pancreatic cancer is just 10.7%, compared to 69% for all cancers overall (AIHW 2024).
Pancreatic cancer is the eighth most common type of cancer in Australia, with around 4,641 new cases diagnosed in 2024 (Cancer Australia 2025). However, it’s becoming more common, possibly due to Australia’s increasing life expectancy (AIHW 2024).
The Pancreas
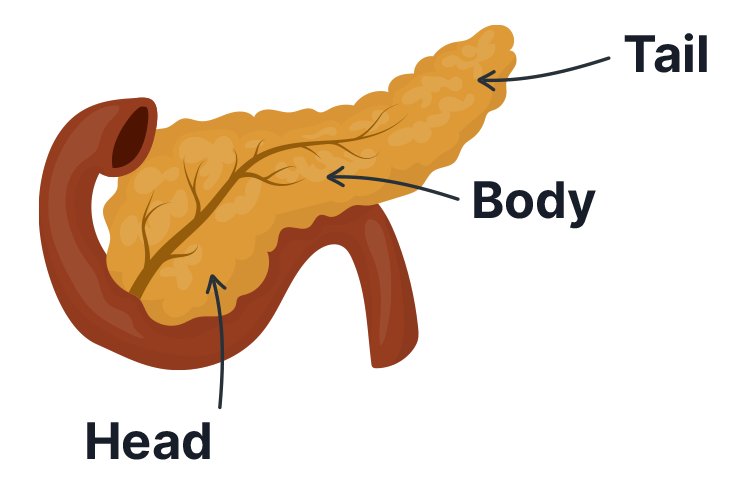
The pancreas is a thin, tadpole-shaped organ. It sits tucked behind the stomach and under the liver, and is part of both the digestive and endocrine systems (Healthdirect 2023; Better Health Channel 2014).
The role of the pancreas in the digestive system is to create and excrete digestive enzymes into the duodenum to help break down partially-digested food. It’s also responsible for secreting sodium bicarbonate to neutralise stomach acid during the digestive process. The portion of the pancreas responsible for digestive tasks is known as the exocrine pancreas (Healthdirect 2023; Better Health Channel 2014).
On the other hand, the endocrine pancreas is responsible for producing the hormones insulin and glucagon, which are used for blood glucose regulation (Better Health Channel 2014).
The pancreas consists of:
- The head (the large, rounded end)
- The body (The middle section)
- The tail (the narrow end).
(Cancer Council 2024)
What is Pancreatic Cancer?
Pancreatic cancer occurs when malignant cells develop in the pancreas. In 70% of cases, cancer is found in the head of the pancreas (Cancer Council 2025).
There are two types of pancreatic cancer:
- Exocrine tumours comprise almost all cases of pancreatic cancer (95%). These are most commonly adenocarcinomas (tumours that develop in exocrine cells lining the pancreatic duct), but can also be adenosquamous carcinomas, acinar cell carcinomas, squamous cell carcinomas or undifferentiated carcinomas.
- Pancreatic neuroendocrine tumours (NETs) are found in the endocrine cells.
(Cancer Council 2024)
Pancreatic cancer has one of the lowest survival rates among all cancers, and is estimated to have the third-highest mortality rate after lung cancer and colorectal cancer (Cancer Australia 2025).
Risk Factors for Pancreatic Cancer
The specific causes of pancreatic cancer are unknown, but identified risk factors include:
- Smoking
- Obesity
- Older age
- Long-time diabetes
- Chronic pancreatitis
- Presence of intraductal papillary mucinous neoplasms (IPMNs) - cysts found in the pancreatic duct
- Helicobacter pylori infection
- Genetic factors (although only 5 to 10% of cases involve a gene mutation that increases the risk of pancreatic cancer)
- Family history of certain genetic conditions (Peutz-Jeghers syndrome, familial breast cancer genes (BRCA1 and BRCA2), familial atypical multiple mole melanoma (FAMMM) syndrome, Lynch syndrome and hereditary pancreatitis)
- Occupational exposure to particular pesticides, dyes or chemicals.
(Cancer Council 2024)
Signs and Symptoms of Pancreatic Cancer
There are often no obvious symptoms in the early stages of pancreatic cancer. In some cases, symptoms may not develop until the cancer has grown large enough to affect other organs or has spread (Cancer Council 2024).
The first noticeable symptom is typically jaundice, which occurs due to a buildup of bilirubin. This can occur if the tumour blocks the common bile duct, allowing bilirubin to accumulate (Cancer Council 2024).

Other possible signs and symptoms include:
- Reduced appetite
- Nausea
- Vomiting
- Unplanned weight loss
- Pain in the upper abdomen, side or back (which may cause the patient to wake up during the night)
- Changes in bowel motions, such as diarrhoea, severe constipation or abnormal stools (pale, oily, foul-smelling and difficult to flush)
- Bloating and increased frequency of flatulence and belching
- New-onset diabetes
- Fatigue.
(Cancer Council 2024)
Note that pancreatic cancer symptoms are often vague, and the condition can present similarly to other conditions (Better Health Channel 2024). Differential diagnoses include pancreatitis, cholangitis (inflammation of the bile duct), cholecystitis (inflammation of the gallbladder), choledochal cyst, peptic ulcer disease, cholangiocarcinoma and gastric cancer (Puckett & Garfield 2024).
Diagnosis of Pancreatic Cancer
Unlike other cancers, such as breast cancer and colorectal cancer, there are no reliable screening tests for pancreatic cancer (Cancer Council 2022).
Instead, patients should be sent for an urgent abdominal CT scan and/or referred to a specialist if they meet one of the following criteria:
| Criteria | Action to be taken |
|---|---|
Patient is over the age of 60 and is experiencing unplanned weight loss in addition to any of the following symptoms:
|
|
| Patient is over the age of 40 and is experiencing jaundice | Referral to a specialist |
Patient has one of the following risk factors that put them at five times the risk of pancreatic cancer:
|
Referral to a specialist |
(Adapted from Loveday et al. 2019)
A suspected diagnosis might be confirmed through:
- Blood test to detect the tumour markers proteins CA 19-9 and CEA
- Imaging (typically a CT scan, but may also include an endoscopic scan, MRI/MRCP scan and/or PET–CT scan)
- Biopsy of the tumour.
(Cancer Council 2024)
Pancreatic Cancer Staging
Pancreatic cancer generally uses the TNM (tumour-nodes-metastasis) staging system (Cancer Council 2024):
| Stage | Description | Percentage of cancers diagnosed at this stage |
|---|---|---|
| Stage I | The cancer is small and can only be found in the pancreas | 20% |
| Stage II | The cancer is large but has not spread outside the pancreas, or is small and has spread to some nearby lymph nodes | |
| Stage III | The cancer has spread to nearby major blood vessels or lots of nearby lymph nodes | 30% |
| Stage IV | The cancer has metastasised to distant areas of the body (e.g. liver, lungs or abdominal lining). It may or may not have spread to the lymph nodes | 50% |
(Cancer Council 2024)
Treatment for Pancreatic Cancer
As a general rule:
- Stage I and II cancers (early pancreatic cancer) can potentially be surgically removed, depending on the patient’s condition.
- Some stage III cancers are borderline resectable, meaning surgical excision is a possibility if other treatment can shrink the cancer first. Others are locally advanced, meaning surgery is not an option, but other treatments can be used to alleviate symptoms.
- Stage IV cancers are metastatic. Surgery is not an option, but other treatments can be used to alleviate symptoms.
(Cancer Council 2024)
Surgical resection (either a Whipple procedure, distal pancreatectomy or total pancreatectomy, depending on the location of the tumour) is the most effective method of treating pancreatic cancer, but unfortunately, most cases are diagnosed too late for surgery to be a viable option (Cancer Council 2024).
In some cases, the patient might need to undergo chemotherapy or chemoradiation prior to the procedure in order to shrink the tumour. Chemotherapy or chemoradiation might also need to be administered after surgery to ensure that any remaining cancer cells are destroyed (Cancer Council 2024).
If surgery is not an option, the patient will receive palliative care to alleviate their symptoms and help them live as comfortably as possible. Palliative care might include:
- Surgery (stenting, bypass surgery, gastroenterostomy or venting gastrostomy) to manage obstruction of the common bile duct or duodenum, which can lead to a variety of symptoms including jaundice, itchiness, loss of appetite, poor digestion, nausea and vomiting
- Chemotherapy, radiation therapy or chemoradiation to slow the growth of the cancer cells
- Pain management via strong analgesics (e.g opioids), nerve blocks, anticonvulsant medicines or complementary therapies
- Referral to a dietitian to improve nutrition
- Antiemetic medicines to alleviate nausea and vomiting
- Diarrhoea management
- Enzyme replacement therapy to aid in digestion
- Diabetes management (if applicable).
(Cancer Council 2024)
Conclusion

Remember that a cancer diagnosis can be highly distressing for patients and their loved ones. When caring for patients with pancreatic cancer, always ensure you provide empathetic care and access to appropriate support where necessary. You should also ensure patients and their families are properly informed about the diagnosis, what symptoms to expect, and what treatment options are available.
Test Your Knowledge
Question 1 of 3
Typically, what is the first noticeable symptom of pancreatic cancer?
Topics
Further your knowledge
 Free
Free
 Free
Free
References
- Australian Institute of Health and Welfare 2024, Cancer Data in Australia: How are Pancreatic Cancer Rates Changing?, Australian Government, viewed 29 May 2025, https://www.aihw.gov.au/reports/cancer/cancer-data-in-australia/contents/cancer-data-commentaries/how-are-pancreatic-cancer-rates-changing
- Better Health Channel 2014, Pancreas, Victoria State Government, viewed 29 May 2025, https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/pancreas
- Better Health Channel 2024, Pancreatic Cancer, Victoria State Government, viewed 29 May 2025, https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/pancreatic-cancer
- Cancer Australia 2025, Pancreatic Cancer in Australia Statistics, Australian Government, viewed 29 May 2025, https://www.canceraustralia.gov.au/cancer-types/pancreatic-cancer/statistics
- Cancer Council 2024, Understanding Pancreatic Cancer, Cancer Council, viewed 29 May 2025, https://www.cancervic.org.au/downloads/booklets/Understanding-Pancreatic-Cancer.pdf
- Cancer Council 2025, Pancreatic Cancer, Cancer Council, viewed 29 May 2025, https://www.cancer.org.au/cancer-information/types-of-cancer/pancreatic-cancer
- Healthdirect 2023, Pancreas, Australian Government, viewed 29 May 2025, https://www.healthdirect.gov.au/pancreas
- Loveday, BPT, Lipton, L & Thomson, BNJ 2019, ‘Pancreatic Cancer: An Update on Diagnosis and Management’, Australian Journal of General Practice, vol. 48, no. 12, viewed 29 May 2025, https://www1.racgp.org.au/ajgp/2019/december/pancreatic-cancer
- Puckett, Y & Garfield, K 2024, ‘Pancreatic Cancer’, StatPearls, viewed 29 May 2025, https://www.ncbi.nlm.nih.gov/books/NBK518996/
 New
New 
