Restrictive Practices: Chemical Restraint in Australia
Published: 29 January 2023
Published: 29 January 2023
‘Human Rights Watch documented several cases in which family members described how relatives with dementia who were taken off medications used to restrain them regained much of their vitality, once again talking and interacting, and staying awake during the day.’
(HRW 2019)
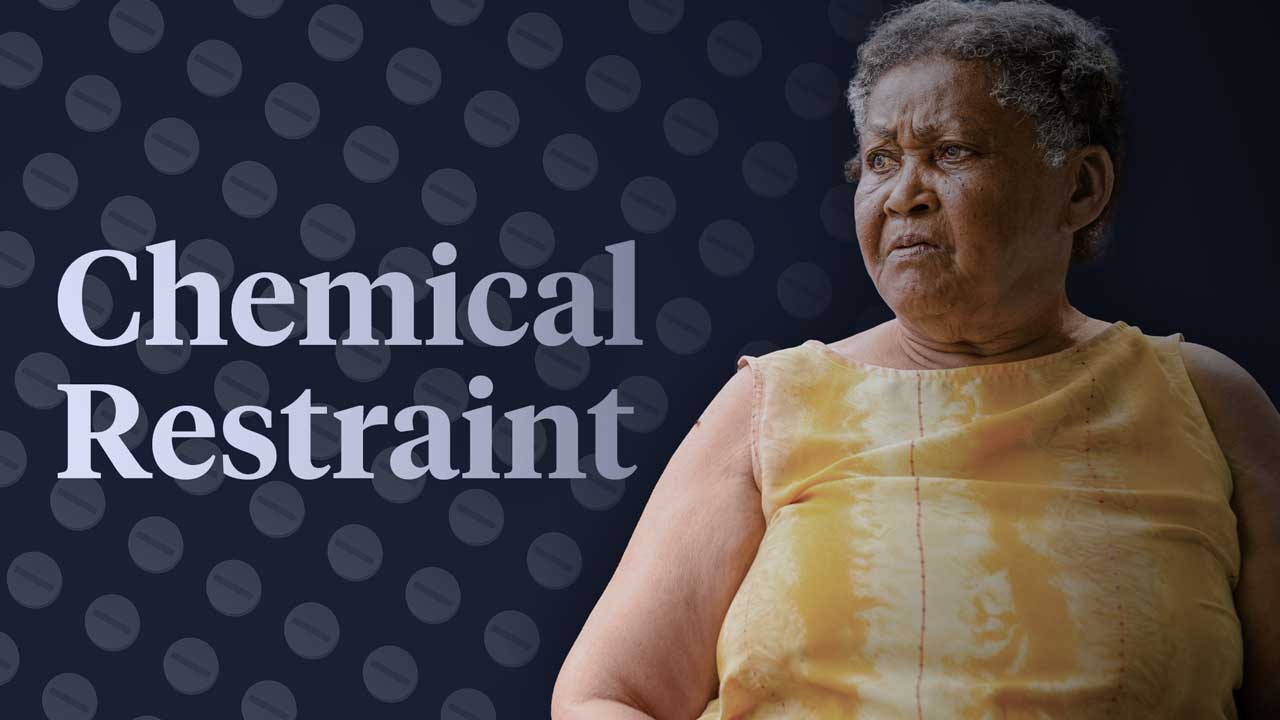
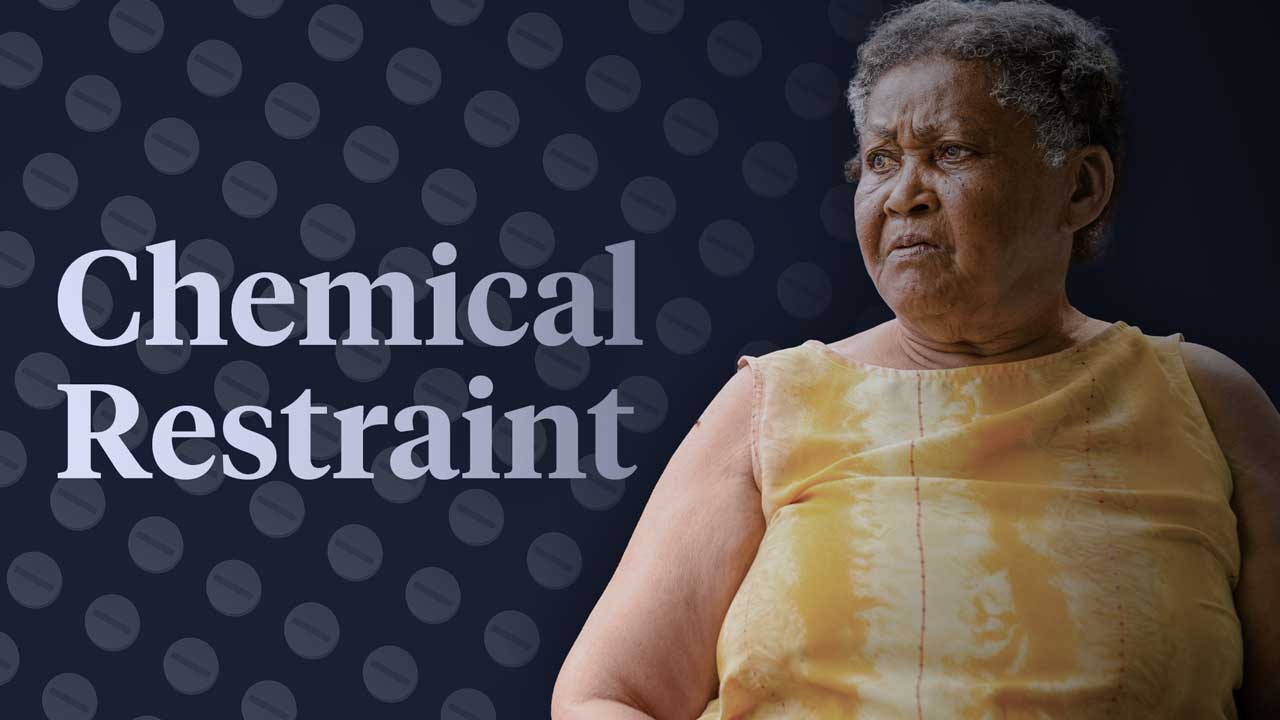
Chemical restraint is the administration of medicine to restrict the movement or decision-making capacity of a person in your care (Dementia Australia 2022).
These medicines, which commonly include psychotropics, anxiolytic/hypnotic agents and antipsychotics, are prescribed for the primary purpose of controlling a person’s behavior. They are not related to the medical treatment of an illness, condition or disorder (Dementia Australia 2022; ACQSC 2021).

Chemical restraint is a form of restrictive practice.
Around the world, including in Australia, older adults are unnecessarily being prescribed antipsychotics in place of behavioural management and proper treatment for underlying conditions (Aged Care Crisis 2015).
In fact, data from the National Aged Care Mandatory Quality Indicator Program has revealed that one in five aged care residents is being given antipsychotic medicines. Yet, half of these people have not been diagnosed with psychosis (Egan 2022).
The Royal Commission into Aged Care Quality and Safety (2019, 2021) identified a ‘clear overuse’ and ‘significant over-reliance’ of chemical restraint in aged care, stating that older adults urgently need to be protected from these ‘unnecessary’ and ‘potentially harmful’ measures.
A Human Rights Watch report released in October 2019, ‘ “Fading Away”: How Aged Care Facilities Chemically Restrain Older People with Dementia’, looked into the use of antipsychotics, benzodiazepines and sedative-hypnotic drugs (known as tranquilisers, sleeping pills or sedatives, and opioid analgesics) as chemical restraints in 35 aged care facilities across Queensland, New South Wales and Victoria.
Through interviews with family members, doctors, nurses and advocates, it uncovered numerous cases of secretive chemical restraint. The author, Bethany Brown, called on the government to ban chemical restraint and to make training compulsory for staff on how to handle the behaviour of residents with dementia.
In many of the case studies featured in the report, family members claimed to have noticed significant and worrying differences in their relatives.
These changes included:
(Brown 2019)
It was ascertained that often, staff did not seek or secure informed consent prior to giving these medications. Many relatives said they only learned of these medications upon receiving pharmacy bills that listed them (Brown 2019).
The HRW report also claimed that those who were taken off chemical restraint medications regained vitality, talked and interacted more, and stayed awake during the day. Unfortunately, others continued to experience the physical and cognitive complications of chemical restraints, such as the loss of muscle strength and the inability to swallow (Brown 2019).
Brown (2019) called for a shift towards person-centred care, citing studies from the United States that found that people with dementia treated with these interventions showed signs of improved quality of life, decreased agitation, improved sleep patterns and improved self-esteem.
There are many well-documented adverse consequences associated with chemical restraint. These include:
(Dementia Australia 2022)
A clinical trial in the US found that antipsychotic drugs increased the risk of death in older people who had dementia. This included benzodiazepines, which were associated with an increased risk of falls, pneumonia and death in older people (Chang 2019).
The HRW report blames understaffing and inadequate training in dementia support for the prominence of chemical restraint in aged care. It claims these factors make it very difficult to take an individualised, comprehensive approach to caring for people with dementia. Therefore, rather than having their needs properly addressed, clients are given medicine to ‘control and subdue’ them. (Brown 2019).

The issue of chemical restraint is timely as the older population of Australia continues to increase.
In 2019 the HRW called for an increase in staffing and regulatory change and enforcement around chemical restraint, making the following key recommendations:
To enact legislation to prohibit the use of chemical restraint as a means of controlling the behaviour of older people (specifically, with dementia) for the convenience of facility staff, as well as:
(Brown 2019)
Breen (2019) notes that it’s important to acknowledge that some residents with behavioural symptoms of dementia might require a low dose of an antipsychotic if they are severely distressed or at risk of causing or incurring harm. Approximately 20% of people with dementia displaying aggressive behaviour will show improvements when prescribed these. However, it’s important that the need for antipsychotic medications is reviewed regularly, with the aim of stopping use.
Legal frameworks around chemical restraint are recent; it was not until July 2019 that regulations around chemical restraint were introduced under the Quality of Care Amendment (Minimising the Use of Restraints) Principles 2019 (HRW 2022).
The Amendment aimed to minimise and prevent the inappropriate use of chemical restraint (and other types of restrictive practices) by establishing that it must only be used as a last resort. However, it did not ban the practice completely (HRW 2022; Kurrle 2021).
In March 2021, the Final Report of the Royal Commission into Aged Care Quality and Safety was released, in which the overuse of restrictive practices was identified as a major problem in Australian aged care facilities (HRW 2022; Kurrle 2021).
In response to recommendations made by the Royal Commission, amendments were made to the Aged Care Act 1997 and Quality of Care Principles 2014 in July 2021. These amendments, which replaced the Quality of Care Amendment (Minimising the Use of Restraints) Principles 2019, expanded upon and strengthened the existing restrictive practice regulations (HRW 2022; DoHAC 2022).
Further amendments to this legislation were made through the Aged Care and Other Legislation Amendment (Royal Commission Response) Act 2022 (DoHAC 2022).
Note: For further information on current restrictive practices legislation, see the Ausmed Training Module Minimising Restrictive Practices in Residential Aged Care.
As of January 2023, chemical restraint is still allowed in Australia but must only be used as a last resort (HRW 2022).
The practice still remains a significant concern, and according to Human Rights Watch (2022), is still widely used across many aged care facilities despite strengthened legislation.
Elaine Pearson, director of Human Rights Watch Australia, has stated that:
‘Policies minimising the use of restraints to modify behaviour are failing to protect older people, showing the need for an outright ban on chemical restraints’ (HRW 2022).

The terminology ‘chemical restraint’ itself carries a stigma. In healthcare, medicines are not commonly referred to as ‘chemicals’. It is not often said that you are ‘chemically relieving a person with asthma,’ but you may hear the phrase ‘chemically restraining a person with dementia’.
By calling psychiatric medicines ‘chemicals’, it differentiates them from other medicines, or implies that agitation deserves punishment or subjugation as opposed to healing (Zeller 2017).
Under international human rights law, governments are obligated to respect the dignity of people living with disability, including older people, by recognising them as being on an equal basis with others. This includes respecting their right to live independently without being made to live in an institution, and to have all their human rights protected if they decide to stay in institutions such as aged care facilities (HRW 2019).
Question 1 of 3
True or false: Understaffing and inadequate training in dementia support may explain the prominence of chemical restraint in Australian aged care.