Asthma is clinically defined as a combination of variable respiratory symptoms such as wheezing, shortness of breath, cough and chest tightness, and significant variation in lung function.
Asthma is a chronic disease that can be controlled but not cured.
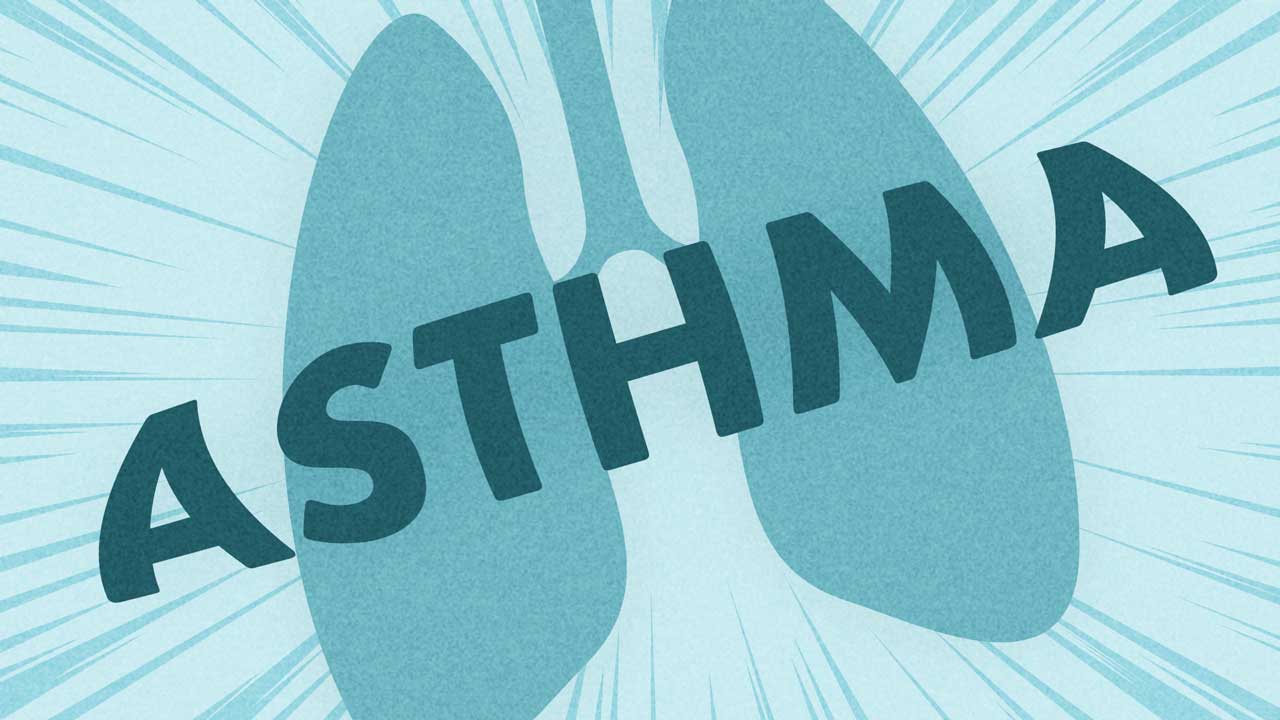
In the event of an asthma attack, triggering stimuli cause the smooth muscles of the bronchi to contract, and consequently, the passage to narrow. The tissue lining of the airway swells as a result of inflammation and secretes mucous (Ortega & Izquierdo 2023). This narrowing of the airways is usually reversible.
A minor asthma attack can be treated at home with proper medications. A severe asthma attack requires medical intervention and has the potential to be a life-threatening emergency.
The most effective way to prevent an asthma attack is to recognise and treat the early signs of an asthma flare-up. To do this, an asthma treatment plan made in collaboration with a general practitioner must be in place and followed (Mayo Clinic 2023).
This plan (detailed below) will detail steps to follow in the event that a person’s asthma worsens and what to do in the event of an asthma attack.

Asthma in Numbers
Roughly 10.8% of Australians have asthma (2.8 million people) (ABS 2023).
The prevalence of asthma among Aboriginal and Torres Strait Islander people is about 1.6 times higher than that of non-First Nations people, and they have almost double the asthma mortality rate of non-First Nations Australians (AIHW 2024).
Asthma is also more common in people residing in lower socio-economic areas and more prevalent in remote areas as opposed to major cities (Asthma Australia 2024a).
Fewer than one in five people over the age of 15 have a written asthma treatment plan, even though it is recommended that every person with asthma have one in place (Asthma Australia 2024b).
Common Asthma Triggers
- Upper respiratory infections such as colds and flu
- Allergens
- Cigarette smoke
- Weather e.g. cold, dry air; thunderstorms; temperature changes
- Exercise
- Certain medicines
- Stress.
(National Asthma Council Australia 2023)
Symptoms of Acute Asthma
- Shortness of breath
- Chest tightness or pain
- Coughing
- Wheezing
- Low peak expiratory flow readings.
(Mayo Clinic 2023)
Most asthma attacks occur in the early hours of the morning. This is generally the time when the effect of protective medicines has worn off and the body is least able to prevent the airway from narrowing (Ortega & Izquierdo 2023).
The symptoms of an asthma attack can vary from person to person (Healthdirect 2022), making it necessary for a person with asthma to work with a healthcare practitioner to identify their unique signs and symptoms.
What Causes Asthma?
The exact cause of asthma is unknown, but is likely a combination of complex interactions between genetics, environmental factors and nutrition (Ortega & Izquierdo 2023).
Diagnosing Asthma
There is no single reliable test to form an asthma diagnosis. Commonly, a diagnosis of asthma is made based on:
- History
- Physical examination
- Consideration of other diagnoses
- Documenting variable airflow limitation.
(National Asthma Council Australia 2023)
Lung Function
Lung (pulmonary) tests evaluate how well a person’s lungs are functioning. Poor lung function indicates that asthma is not currently well-controlled (Mayo Clinic 2023).
Lung function tests include:
- Peak flow: This test measures how quickly a person can breathe out - known as peak expiratory flow (PEF). A peak flow test is performed by blowing into a mouthpiece as hard and as fast as possible in one breath.
- Spirometry: During spirometry, a person takes deep breaths and forcefully exhales into a hose connected to a machine called a spirometer. A typical spirometry measurement is forced expiratory volume, measuring how fast a person can breathe out in one second.
- Nitric oxide measurement: This measures the amount of nitric oxide gas a person has in their breath when they exhale. High nitric oxide readings indicate that a person’s bronchial tubes are inflamed.
- Pulse oximetry: A test that measures the amount of oxygen in the person’s blood; this is measured through the fingernails.
(Mayo Clinic 2023)
When to Seek Emergency Medical Treatment
It’s recommended that a person seeks immediate medical attention if:
- Their symptoms are worsening quickly
- They are experiencing severe breathlessness, can’t speak properly or have blue lips
- Symptoms are not improving after using a quick-acting (rescue) inhaler.
(National Asthma Council 2022)
Asthma Action Plans
An individualised written asthma action plan is necessary for people with asthma. It will be made in accordance with their treatment regimen, the severity of their asthma, their culture, language and ability to self-manage.
An asthma action plan should include the following:
- The person’s usual asthma medicines and dosages
- Instructions on what to do when asthma symptoms worsen (e.g. when to increase dosages, when to escalate care)
- Information on what to do during an asthma emergency
- The name of the healthcare professional who developed the plan
- The date the plan was made/updated.
(National Asthma Council 2022)
Treating Asthma
Medicines used to treat asthma allow people to live normal lives. In many cases, the medicines used to treat an asthma attack can be used (in lower doses) to limit the occurrence of attacks.
For a comprehensive list of all asthma medicines in Australia, see the National Asthma Council’s Asthma & COPD Medications chart.
Preventing Asthma
It’s strongly advised that people who have asthma learn their triggers and do their best to avoid them.
Other prevention tips include:
- Having an adequate supply of medications and always following the instructions when using them
- Informing a general practitioner when medications are less effective or aren’t working
- Paying attention to symptoms in the event of a cold or flu
- Seeking medical help immediately if an acute exacerbation is a possibility.
(Pietrangelo & Sullivan 2019)
Test Your Knowledge
Question 1 of 3
Which one of the following is a symptom of acute asthma?
Topics
Further your knowledge
 Free
Free Free
Free Free
Free Free
Free
References
- Asthma Australia 2024a, Asthma Statistics & Facts, Asthma Australia, viewed 17 January 2025, https://asthma.org.au/what-is-asthma/statistics/
- Asthma Australia 2024b, What is Asthma?, Asthma Australia, viewed 17 January 2025, https://asthma.org.au/asthma/
- Australian Bureau of Statistics 2023, Asthma, Australian Government, viewed 17 January 2025, https://www.abs.gov.au/statistics/health/health-conditions-and-risks/asthma/latest-release
- Australian Institute of Health and Welfare 2024, First Nations People with Asthma, Australian Government, viewed 17 January 2025, https://www.aihw.gov.au/reports/chronic-respiratory-conditions/chronic-respiratory-conditions/contents/first-nations-people-with-asthma
- Healthdirect 2022, Asthma, Australian Government, viewed 17 January 2025, https://www.healthdirect.gov.au/asthma
- Mayo Clinic 2023, Asthma Attack, Mayo Clinic, viewed 17 January 2025, https://www.mayoclinic.org/diseases-conditions/asthma-attack/symptoms-causes/syc-20354268
- National Asthma Council Australia 2022, Australian Asthma Handbook, National Asthma Council Australia, viewed 17 January 2025, https://www.asthmahandbook.org.au/
- National Asthma Council Australia 2023, What are Asthma Triggers?, National Asthma Council Australia, viewed 17 January 2025, https://www.nationalasthma.org.au/understanding-asthma/what-are-asthma-triggers
- Ortega, V E & Izquierdo, M 2023, Asthma, MSD Manual, viewed 17 January 2025, https://www.msdmanuals.com/en-au/home/lung-and-airway-disorders/asthma/asthma
- Pietrangelo, A & Sullivan, D 2019, ‘Acute Exacerbation of Asthma’, Healthline, 8 March, https://www.healthline.com/health/asthma/acute-asthma-exacerbation
 New
New