A patient who requires prolonged mechanical ventilation, is experiencing upper airway obstruction or needs assistance with chronic airway secretions may undergo a tracheostomy (Raimonde et al. 2023).
What is a Tracheostomy?
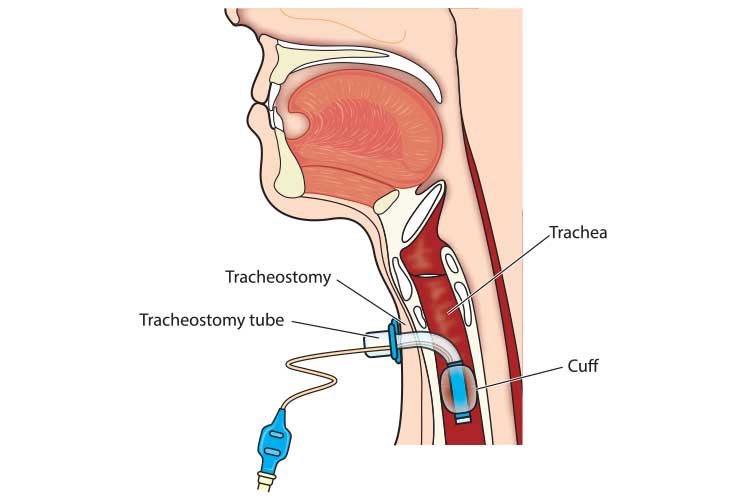
A tracheostomy is a surgical procedure that involves making an incision (stoma) into the trachea through the front of the neck. A tube is then inserted into the incision, creating an air passage that allows the patient to breathe directly through their trachea while avoiding their upper airway. This may be a temporary or permanent intervention (Healthdirect 2021; Mayo Clinic 2019).
It is vital to ensure you care for a tracheostomy carefully and thoroughly, as an adverse event such as respiratory distress may develop if the tracheostomy is not managed properly.

Indications for a Tracheostomy
The most common reasons for undergoing a tracheostomy are:
- Managing an upper-airway obstruction (caused by a tumour, surgery, foreign body or infection)
- Preventing damage to the larynx and upper airways after prolonged trans-laryngeal intubation
- Providing easy access to the lower airway for suctioning and the removal of secretions
- Providing a stable airway for a patient who requires prolonged mechanical ventilation or oxygenation support.
(CCAM 2016)
Conditions that may lead to a tracheostomy being required include:
- Neurological conditions (e.g. stroke)
- Severe head or neck injury
- Spinal injury
- Burns
- Severe pneumonia
- Acquired or congenital subglottic stenosis
- Anaphylaxis
- Head or neck cancer
- Radiation therapy to the head or neck
- Severe lung disease
- When an endotracheal tube has been in situ for more than seven days, a tracheostomy may be considered.
(Healthdirect 2021)
Types of Tracheostomy Tubes
There are a variety of tracheostomy tubes available with some or all of the following features, depending on what the patient requires:
- An inner cannula is a small tube inserted into the larger outer tube. It can be removed for cleaning while the outer tube stays in situ, helping to prevent mucus build-up.
- A cuff is a balloon on the outside of the tube, which inflates and creates an airtight seal against the airway walls. It prevents air from escaping through the nose and mouth and can also prevent the aspiration of saliva. Mechanically ventilated patients with tracheostomies require cuff inflation.
- An obturator/introducer attaches to the tracheostomy tube, creating a smooth, round tip. It is only used during the insertion of a tube to prevent damage to the trachea. It should be removed and discarded after tube insertion.
- Fenestrations are small holes on the upper surface of the tube that allow air and secretions to pass into the upper airways. Fenestrations help to facilitate speech, however, care should be taken to ensure they do not become blocked by downward-passing secretions.
- Sub-glottic suction ports facilitate suctioning above the cuff to prevent secretions from accumulating and going into the patient’s airway.
(ACI 2021; Dawson 2014; Craig Hospital 2014; CCAM 2016)
Caring for a Tracheostomy
Caring for a tracheostomy might include:
- Ensuring there is a tracheostomy emergency kit available in the patient’s room at all times and that the equipment inside is checked on the commencement of each shift. Follow local policy and procedures. This is essential.
- Monitoring the patient’s skin condition, maintaining the cleanliness of the incision (stoma) area and changing dressings.
- Performing routine suctioning to ensure the patient’s airways remain patent.
- Monitoring and reporting abnormal secretions.
- Donning appropriate PPE (googles, gown, gloves, mask) when caring for and suctioning the patient.
- Cleaning and maintaining suctioning equipment.
- Supporting routine tube tie changes.
- Keeping appropriate charts and records.
- Identifying and responding to the signs of airway obstruction.
- Implementing emergency procedures related to patient deterioration or infection.
- Adequately humidifying the trachea to prevent thick mucus and tube blockage.
- Cuff management and cuff pressure monitoring.
- Oral hygiene assessments.
- Maintaining the cleanliness and patency of the inner cannula.
- Establishing a non-verbal communication system for patients who are not able to achieve verbal speech.
- Monitoring and assisting with swallowing.
- Preparing the patient for and performing weaning and decannulation from the tracheostomy.
- Assisting the medical and/or surgical team with tube changing.
- Ensuring the patient has cooling devices (e.g. cold wet face washer on the forehead, light bed linen, frequent washes), as the humidification attached to the tracheostomy can make them feel hot.
(NDIS 2022; Karaca 2016; ACI 2021; Dawson 2014)
Tracheostomy Complications
Early Complications
Although complications during placement are uncommon, they can be serious (Fernandez-Bussy et al. 2015).
Early complications are defined as those that occur within the first postoperative week (RCHM 2022). They may include:
- Haemorrhage
- Pneumothorax
- Subcutaneous emphysema
- Cuff leak
- Respiratory or cardiac collapse
- Infection of the stoma
- Tube dislodgement
- Tube occlusion (e.g. from build-up of secretions)
- Formation of stomal or tracheal granulation tissue
- Stomal erosion
- Fistulae.
(RCHM 2022; Raimonde et al. 2023)
Late Complications
Late complications become more likely the longer the tube is kept in situ and are estimated to affect about 65% of patients. Patients who are critically ill or have comorbidities are more at risk (Fernandez-Bussy et al. 2015). These complications may include:
- Tube obstruction
- Tube occlusion
- Tube dislodgement
- Fistulae
- Infection
- Aspiration
- Tracheal trauma
- Tracheal stenosis
- Tracheomalacia
- Skin breakdown or pressure injury around the stoma.
(RCHM 2022)
Tracheostomy Emergency Management
Being able to identify the following signs of respiratory distress is crucial in promptly and appropriately addressing an emergency situation.
| Signs of Respiratory Distress | Possible Causes of Respiratory Distress |
|---|---|
|
|
(RCHM 2022; SESLHD 2020)
In the case of respiratory distress, you should take these immediate steps:
- Call for assistance.
- Provide 100% high flow oxygen via tracheostomy or face mask. Manually ventilate if required with a bag- valve mask (BVM) apparatus.
- Check the oxygen source and connections, cuff inflation and humidifier.
- If an inner cannula is in situ, check to see if there is a blockage and change it if required.
- Conduct a head-to-toe assessment. Reassure the patient.
- Check the positioning of the patient’s head/neck and the tracheostomy tube. If required, realign the tube to the midline.
- If the tube is dislodged, maintain a patent airway (through head/neck positioning, jaw thrust and/or artificial oropharyngeal airway). Only an appropriately trained staff member may insert a new tube.
- If the tube is still in situ but obstruction is suspected:
- Pass a suction catheter and apply suction.
- Change the inner cannula if present (ideally with a non-fenestrated one).
- If the tube is obstructed, deflate the cuff if one is present.
- Monitor the patency of the tube, the presence of any secretions and whether the patient is responding to suction.
- If the patient’s respiratory distress reduces, assess if airflow is present and unobstructed and whether oxygen is adequate. A clinical assessment should be performed to identify the cause of the distress.
- Perform chest auscultation assessment to ensure there is equal air entry to both sides of the lungs.
- If there is no airflow through or around the tube:
- Insert tracheal dilators around the tube into the stoma.
- Remove the tube.
- Insert a bougie or suction catheter. This must only be performed by an expert clinician with relevant experience.
- Maintain an oropharyngeal airway to achieve oxygenation.
- If a laryngectomy patient, focus on clearing the stoma and trachea.
(SESLHD 2020)

Emergency Bedside Equipment
All tracheostomy patients should have the following equipment accessible by their bedside at all times in the event of an emergency:
- Tracheostomy checklist
- Humidifier (set at 37 degrees)
- Suction catheters
- Clean gloves
- Yankauer sucker
- Cuff manometer and a 10 ml syringe
- Tracheal dilators
- Bag mask valve apparatus (with tracheostomy connecter and face mask)
- Syringe
- Spare tracheostomy tubes (one the same size as the tube in situ and another that is one size smaller)
- Water (for cleaning suction tubing)
- Waste disposal bag
- Suction canister, tubing and suction device
- Tracheostomy dressings
- Tracheostomy tapes
- Protective eyewear
- Bottle of sterile water to clean suction tubing after use.
(Austin Health 2021)
Conclusion
Tracheostomies can be both temporary and permanent and may appear in a variety of care and clinical settings. Being able to thoroughly monitor and care for tracheostomies is essential in preventing complications.
Note: This article is intended as a refresher and should not replace best-practice care. Always refer to your facility's policy on tracheostomy care and emergency management.
Test Your Knowledge
Question 1 of 3
What is the definition of an early complication?
Topics
References
- Agency for Clinical Innovation 2021, Care of Adult Patients in Acute Care Facilities With a Tracheostomy, New South Wales Government, viewed 19 June 2023, https://aci.health.nsw.gov.au/networks/icnsw/clinicians/acute-tracheostomy
- Austin Health 2021, Mandatory Tracheostomy Equipment, Austin Health, viewed 19 June 2023, https://tracheostomyteam.org/wp-content/uploads/2023/02/MANDATORY-TRACHEOSTOMY-EQUIPMENT-EMERGENCY-TRACHEOSTOMY-MANAGEMENT-POSTER.pdf
- Critical Care Airway Management 2016, Tracheostomy, CCAM, viewed 19 June 2023, https://www.ccam.net.au/handbook/tracheostomy/
- Craig Hospital 2014, Tracheostomy Guide, Craig Hospital, viewed 19 June 2023, https://craighospital.org/resources/tracheostomy-guide
- Dawson, D 2014, ‘Essential Principles: Tracheostomy Care in the Adult Patient’, British Association of Critical Care Nurses, vol. 19, no. 2, viewed 19 June 2023, https://healthhealingj4uo.trubox.ca/wp-content/uploads/sites/579/2018/11/Dawson-2014-Nursing_in_Critical_Care.pdf
- Fernandez-Bussy et al. 2015, 'Tracheostomy Tube Placement', Journal of Bronchology & Interventional Pulmonology, vol. 22, no. 4, viewed 15 June 2020, https://journals.lww.com/bronchology/Fulltext/2015/10000/Tracheostomy_Tube_Placement__Early_and_Late.19.aspx
- Healthdirect 2021, Tracheostomy, Australian Government, viewed 19 June 2023, https://www.healthdirect.gov.au/tracheostomy
- Mayo Clinic 2019, Tracheostomy, Mayo Clinic, viewed 19 June 2023, https://www.mayoclinic.org/tests-procedures/tracheostomy/about/pac-20384673
- NDIS Quality and Safeguards Commission 2022, NDIS Practice Standards: Skills Descriptors, Australian Government, viewed 19 June 2023, https://www.ndiscommission.gov.au/sites/default/files/2022-12/Revised%20High%20Intensity%20Support%20Skills%20Descriptors.pdf
- Karaca, T 2016, ‘Nursing Care: Basic Principles of Tracheostomy Care at Home’, International Journal of Advanced Research, vol. 4, no. 6, viewed 19 June 2023, https://www.researchgate.net/publication/305413313_NURSING_CARE_BASIC_PRINCIPLES_OF_TRACHEOSTOMY_CARE_AT_HOME
- Raimonde, AJ, Westhoven, N & Winters, R 2023, ‘Tracheostomy’, StatPearls, viewed 19 June 2023, https://www.ncbi.nlm.nih.gov/books/NBK559124/
- Royal Children’s Hospital Melbourne 2022, Tracheostomy Management, Royal Children’s Hospital Melbourne, viewed 19 June 2023, https://www.rch.org.au/rchcpg/hospital_clinical_guideline_index/Tracheostomy_Management_Guidelines/#Complications
- South Eastern Sydney Local Health District 2020, Tracheostomy Clinical Management Procedures for Adult Inpatients, New South Wales Government, viewed 19 June 2023, https://www.seslhd.health.nsw.gov.au/sites/default/files/documents/SESLHDPR%20298%20-%20Tracheostomy%20Clinical%20Management%20Procedures%20for%20Adults%20Inpatients_0.pdf
 New
New