Transient ischaemic attacks (TIAs), sometimes referred to as ‘mini strokes’, are often ignored because symptoms improve and the immediate effects are minimal. However, they are a warning sign that must be taken seriously (American Stroke Association 2019).
What is a Transient Ischaemic Attack?
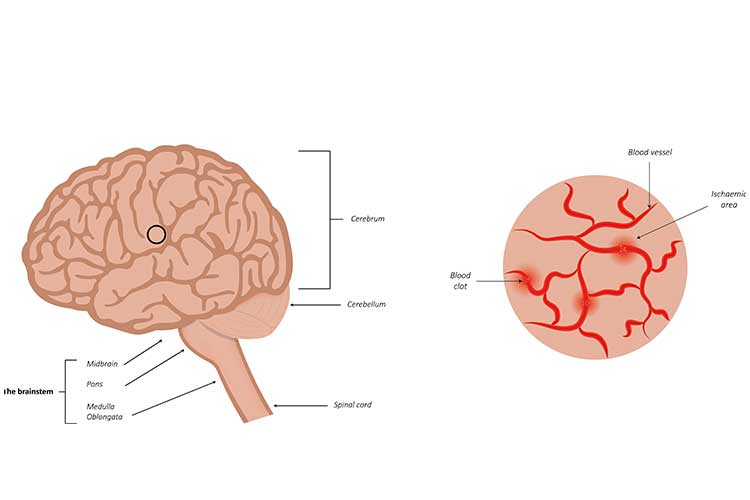
A transient ischaemic attack (TIA) is essentially a minor stroke that often lasts for a short duration of time. It is caused by a temporary blockage of the blood supply to the brain, starving it of oxygen and nutrients (Stroke Foundation 2023).
Unlike a stroke, where the prolonged blockage causes brain cells to die and results in permanent damage, a TIA will generally resolve after only a few minutes (though it may last for up to 24 hours). This allows the oxygen and nutrients to quickly return to the brain, and the patient will fully recover with no lasting effects (Stroke Foundation 2023; American Stroke Association 2019).
However, a TIA can be a warning that a full-blown stroke is imminent. For this reason, TIAs should be treated as an emergency and should never be ignored (American Stroke Association 2019).
What is the Risk of Stroke After a TIA?
Approximately one in three people who experience a TIA will go on to have a stroke (Mayo Clinic 2022).
The patient’s risk of stroke is highest in the first few hours and days after the TIA (Stroke Foundation 2023), but a stroke can occur months or even years later. About half of all eventual strokes will occur within the first year following the TIA (Mayo Clinic 2022).
There is increased risk of a stroke following a TIA if:
- The TIA lasted for longer than 10 minutes
- The patient experienced unilateral weakness and/or speech difficulties during the TIA
- The patient is over 60 years old
- The patient’s blood pressure upon first evaluation was at or above 140/90 mmHg
- The patient has diabetes.
(Panuganti et al. 2022)
Risk Factors for a TIA
- Age (people over 55 are at increased risk)
- Sex (men are at slightly increased risk)
- Family history of TIA or stroke
- Previous TIA
- High blood pressure (over 140/90 mmHg) or cholesterol
- Cardiovascular disease
- Artery disease
- Diabetes
- High levels of homocysteine
- Obesity
- Smoking
- Lack of exercise
- Poor diet
- Heavy alcohol consumption
- Illicit drugs
- COVID-19 infection.
(Mayo Clinic 2022)
Signs of a TIA
The symptoms of a TIA are virtually identical to those of a stroke, but will generally resolve within an hour. They include:
- Severe, sudden headache
- Vision disturbances (e.g. loss of vision in one or both eyes, double vision)
- Speech disturbances (e.g. using the wrong words)
- Slurred speech
- Facial numbness or weakness
- Difficulty swallowing
- Weakness, paralysis or tingling of the face, arms or legs
- Vertigo
- Loss of balance
- Nausea and vomiting.
(Healthdirect 2022)
Remember the FAST test:
| F (Face) | Has the patient’s face drooped? |
| A (Arms) | Can the patient lift both arms? |
| S (Speech) | Is the patient’s speech slurred or confused? Can they understand you? |
| T (Time) | Time is critical. Any of these signs could indicate a stroke. |
(Stroke Foundation 2023)

Treating a TIA
When a patient experiences a TIA, the primary goal is to prevent a stroke from occurring.
- At the onset of a TIA:
- Escalate care
- Conduct a head-to-toe assessment
- Ensure the patient is safe
- Reassure the patient
- Increase the frequency of observation (neurological assessment and vital signs)
- Commence basic life support if the patient is unresponsive
- Coordinate diagnostic testing
- Clearly document the patient’s signs and symptoms
- The patient should undergo a full assessment to confirm the incidence of a TIA. This may include:
- Brain scan
- Magnetic resonance imaging (MRI)
- Computerised tomography (CT) scan
- Heart tests
- Electrocardiogram (ECG)
- Echocardiogram (ECHO)
- Artery tests
- Ultrasound
- CT scan
- Magnetic resonance angiogram (MRA)
- Blood tests
- Blood pressure
- Brain scan
- The patient should commence anticoagulation therapy as soon as possible (if haemorrhage has been excluded and there are no containdications).
- Lifestyle risk factors should be identified and modified. These may include:
- Smoking cessation
- Improving diet
- Increasing exercise
- Limiting alcohol
- Other inventions may include:
- Blood pressure-lowering therapy
- Cessation of hormone replacement therapy
- Diabetes management
- Antiplatelet therapy
- Lipid-lowering medicines
- If the occlusion is greater than 70%, the patient may undergo carotid endarterectomy surgery to remove plaque from the carotid artery.
- Ensure education about driving is delivered by the medical practitioner before the patient is discharged - in most cases, the ptient won’t be able to drive for two weeks after a TIA.
(Stroke Foundation 2022, 2023; Better Health Channel 2022)
Preventing TIAs
The following lifestyle changes may be able to prevent the likelihood of experiencing a TIA or stroke:
- Refraining from smoking
- Limiting cholesterol and fat
- Maintaining a healthy diet
- Limiting sodium intake
- Exercising regularly
- Limiting alcohol consumption
- Maintaining a healthy weight
- Avoiding illicit drugs
- Managing underlying conditions such as diabetes, high cholesterol, high blood pressure or atrial fibrillation.
(Mayo Clinic 2022; NHS 2020)

Conclusion
Early detection and prompt treatment of a patient who has experienced a TIA is imperative in ensuring the best outcome and reducing the likelihood of stroke. Remember to escalate care if a patient is demonstrating the signs and symptoms of a TIA or stroke.
Note: This article is intended as a refresher and should not replace best-practice care. Always refer to your facility's policy on stroke and TIA management.
Test Your Knowledge
Question 1 of 3
True or false: The signs of a TIA are virtually identical to those of a stroke.
Topics
References
- American Stroke Association 2010, TIA (Transient Ischemic Attack), American Heart Association, viewed 5 June 2023, https://www.stroke.org/en/about-stroke/types-of-stroke/tia-transient-ischemic-attack
- Better Health Channel 2022, Transient Ischaemic Attack (TIA), Victoria State Government, viewed 5 June 2023, https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/transient-ischaemic-attack-tia
- Healthdirect 2022, Transient Ischaemic Attack (TIA), Australian Government, viewed 5 June 2023, https://www.healthdirect.gov.au/transient-ischaemic-attack-tia
- Mayo Clinic 2022, Transient Ischaemic Attack (TIA), Mayo Clinic, viewed 5 June 2023, https://www.mayoclinic.org/diseases-conditions/transient-ischemic-attack/symptoms-causes/syc-20355679
- National Health Service 2020, Transient Ischaemic Attack (TIA): Prevention, NHS, viewed 5 June 2023, https://www.nhs.uk/conditions/transient-ischaemic-attack-tia/prevention/
- Panuganti, KK, Tadi, P & Lui, F 2022, ‘Transient Ischemic Attack’, StatPearls, viewed 5 June 2023, https://www.ncbi.nlm.nih.gov/books/NBK459143/
- Stroke Foundation 2022, Australian and New Zealand Clinical Guidelines for Stroke Management, Stroke Foundation, viewed 5 June 2023, https://informme.org.au/guidelines/living-clinical-guidelines-for-stroke-management
- Stroke Foundation 2023, Transient Ischaemic Attack (TIA), Stroke Foundation, viewed 5 June 2023, https://strokefoundation.org.au/media/mb2e41ae/tia-brochure.pdf
 New
New