Vasa praevia is a rare condition that may result in a catastrophic haemorrhage in the fetus.
What is Vasa Praevia?
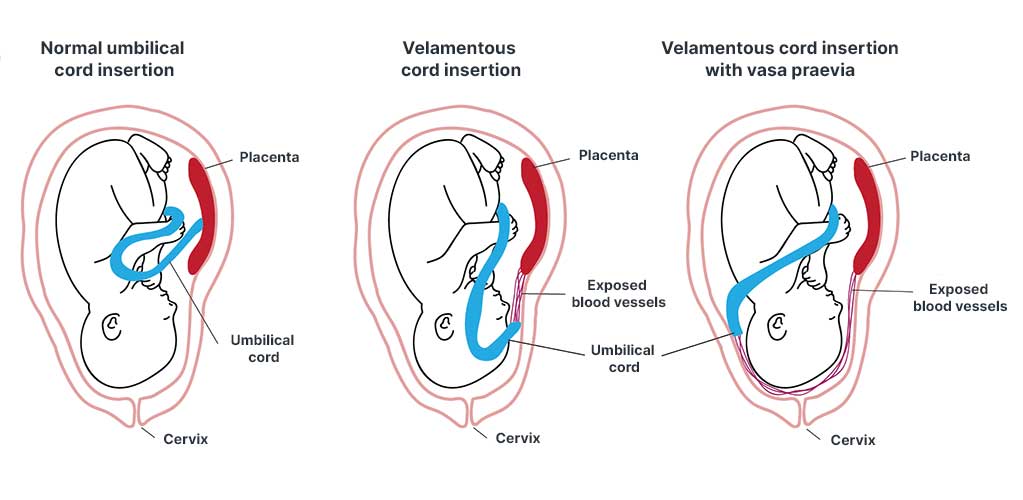
The blood vessels between the fetus and placenta (umbilical vessels) are usually contained in the umbilical cord (Dulay 2024).
However, in vasa praevia, some of these umbilical vessels are instead located outside of the umbilical cord in the membranes surrounding the fetus, near the cervical opening (Dulay 2024).
Following either spontaneous or artificial rupture of the membranes, these delicate vessels may tear, potentially causing fetal exsanguination (RCOG 2018; Sullivan et al. 2017).
Vasa praevia often coexists with a velamentous insertion of the umbilical cord or a low-lying placenta. It is associated with a high perinatal mortality rate of over 60% if not detected before labour (Sullivan et al. 2017).
Two types of vasa praevia are commonly recognised:
- Type one occurs when the vessel is connected to a velamentous umbilical cord
- Type two occurs when the vessel connects the placenta with a succenturiate or accessory lobe
(Jauniaux et al. 2018)
How Common is Vasa Praevia?
Although published statistics seem to vary quite widely, Sullivan et al. (2017) estimate that the incidence of patients with vasa praevia in Australia is approximately 6 to 11 cases per 10,000 pregnancies. Sutera et al. (2021) also suggest a global incidence between 1 in 500 to 1 in 5,000 pregnancies. All of these statistics are tragically high and point to the need to detect vasa praevia before the onset of labour, allowing time for an elective caesarean birth to be arranged.
Risk Factors for Vasa Praevia
As Sutera et al. (2021) suggest, around 85% of cases of vasa praevia can be detected early through the presence of velamentous cord insertion or a low-lying placenta.
Sullivan et al. (2017) also make the point that known risk factors such as multiple pregnancy and in vitro fertilisation are becoming increasingly common in high-income countries characterised by an ageing reproductive population and greater use of assisted reproductive technology.
Approximately 85% of cases of vasa praevia have one or more identifiable risk factors, including:
- In vitro fertilisation
- Multiple gestations
- Bilobed placenta
- Succenturiate lobe
- Low-lying placenta
- Velamentous cord insertion
(Melcer et al. 2018)
Early Diagnosis is Essential
Early diagnosis of vasa praveia and elective caesarean birth are essential to mitigate the risk of perinatal death (Sullivan et al. 2017).
The key to improving fetal survival is avoiding either artificial or spontaneous rupture of the membranes. This is extremely important because the entire fetal cardiac output passes through the umbilical cord and it can take less than 10 minutes for total exsanguination of the fetus to occur (Datta et al. 2015).
As Jauniaux et al. (2018) have found, once the membranes have ruptured, the fetal mortality rate is at least 60% even if an emergency caesarean birth is initiated. In comparison, a survival rate of over 95% was found in cases where ultrasound diagnosis was made antenatally, allowing time to plan an elective caesarean birth.
In other words, prenatal diagnosis is the key to improved fetal survival.
Screening for Vasa Praevia

According to guidelines from the Royal Australian and New Zealand College of Obstetricians and Gynaecologists (RANZCOG):
- Routine screening for vasa praevia using a transvaginal scan is not recommended in singleton pregnancies
- Where possible, placental cord insertion should be documented during the routine mid-trimester scan using a transvaginal scan and colour Doppler
- Screening using a transvaginal scan is recommended for patients with risk factors associated with vasa praevia, including:
- Velamentous cord insertion
- Succenturiate lobe
- Placenta praevia
- IVF pregnancy
(RANZCOG 2019)
Midwifery Management
For midwives, confident and rapid diagnosis can increase the chances of a successful outcome. For example, if initial fetal heart rate tracings are concerning, steps should be taken to prepare for an emergency caesarean birth with appropriate neonatal resuscitation immediately available.
Lack of clinical knowledge and outdated policies are often cited as areas for improvement, along with the need for updated research. Yet, this is made difficult due to the rare nature of this condition.
Hospitalisation in the third trimester is generally recommended for patients with vasa praevia as it allows access to emergency caesarean birth in the case of unexpected rupture of the membranes (Sullivan et al. 2017). Outpatient management is also considered possible as long as there is no evidence of cervical shortening on ultrasound, and there are no symptoms of bleeding or uterine contractions. Most patients then go on to deliver by elective caesarean birth between 34 and 36 weeks gestation (Melcer et al. 2018).
How should patients with vasa praevia be managed in labour? The answer, according to Jauniaux et al. (2018), is to move to an emergency caesarean birth even before the diagnosis is confirmed because of the speed at which fetal exsanguination can occur, as well as the high perinatal mortality rate associated with this condition.
In an ideal situation, delivery should be delayed if it’s safe to do so (before the rupture of the membranes) in order to minimise the impact of iatrogenic prematurity. Generally, this is achieved with the administration of corticosteroids for fetal lung maturity from 32 weeks gestation, with delivery planned for 34 to 36 weeks gestation (RANZCOG 2019).
Conclusion
Vasa praevia is rightly referred to as an avoidable obstetric tragedy. Today, as midwifery services continue to improve and local protocols evolve to reflect the latest research, it is more likely than ever that antenatal screening will be used to detect the presence of vasa praevia before the onset of catastrophic bleeding, hopefully saving the lives of many infants.
As Javid et al. (2019) note, midwives have a critical role in caring for and supporting patients with vasa praevia. Continuing to improve midwives’ knowledge using contemporary evidence and clinical guidelines should enable them to deliver safer maternity care and improve a patient’s journey through this potentially catastrophic condition.
Topics
References
- Datta, S, Babu, KM, Mitra, S & Patil, D 2015, ‘Vasa Previa: An Avoidable Obstetric Tragedy’, J Obstet Gynaecol India., vol. 66, no. 3, viewed 15 June 2024, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4870668/
- Dulay, A T 2024, Vasa Previa, MSD Manual, viewed 15 July 2024, https://www.msdmanuals.com/en-au/home/women-s-health-issues/complications-of-pregnancy/vasa-previa
- Jauniaux, ERM, Alfirevic, Z, Bhide, AG, Burton, G J, Collins, SL & Silver, R 2018, ‘Vasa Praevia: Diagnosis and Management’, BJOG: An International Journal of Obstetrics & Gynaecology, vol. 126, no. 1, viewed 15 June 2024, https://obgyn.onlinelibrary.wiley.com/doi/full/10.1111/1471-0528.15307
- Javid, N, Hyett, J & Homer, C 2019, ‘Providing Quality Care for Women With Vasa Praevia: Challenges and Barriers Faced by Australian Midwives’, Midwifery, vol. 68, viewed 15 June 2024, https://www.sciencedirect.com/science/article/abs/pii/S0266613818303085
- Melcer, Y, Maymon, R & Jauniaux, E 2018, ‘Vasa Previa: Prenatal Diagnosis and Management’, Current Opinion in Obstetrics & Gynecology, vol. 30, no. 6, viewed 15 June 2024, https://journals.lww.com/co-obgyn/abstract/2018/12000/vasa_previa__prenatal_diagnosis_and_management.8.aspx
- Royal Australian and New Zealand College of Obstetricians and Gynaecologists 2019, Vasa Praevia, RANZCOG, viewed 15 July 2024, https://ranzcog.edu.au/wp-content/uploads/2022/05/Vasa-Praevia.pdf
- Royal College of Obstetricians and Gynaecologists 2018, Placenta Praevia, Placenta Accreta and Vasa Praevia, RCOG, viewed 15 July 2024, https://www.rcog.org.uk/en/patients/patient-leaflets/placenta-praevia/
- Sullivan, E, Javid, N, Duncombe, G, Li, Z, Safi, N, Cincotta, R, Homer, C, Halliday, L & Oyelese, Y 2017, ‘Vasa Previa Diagnosis, Clinical Practice, and Outcomes in Australia’, Obstetrics & Gynecology, vol. 130, no. 3, viewed 15 June 2024, https://journals.lww.com/greenjournal/Fulltext/2017/09000/Vasa_Previa_Diagnosis,_Clinical_Practice,_and.14.aspx
- Sutera, M, Garofalo, A, Pilloni, E, Parisi, S, Alemanno, M, Menato, G, Sciarrone, A & Viora, E 2021, ‘Vasa Previa: When Antenatal Diagnosis can Change Fetal Prognosis’, Journal of Perinatal Medicine, viewed 15 June 2024, https://www.degruyter.com/document/doi/10.1515/jpm-2020-0559/html
 New
New 
