In Australia, breast cancer is the most common type of cancer affecting women apart from non-melanoma skin cancer, with about one in seven women expected to be diagnosed with breast cancer during their lifetime (Cancer Council Victoria 2022).
It’s also possible, albeit rare, for breast cancer to affect men, with about 160 men diagnosed every year. Trans women, trans men, non-binary and gender-diverse people may also be at risk (Cancer Council Victoria 2022).
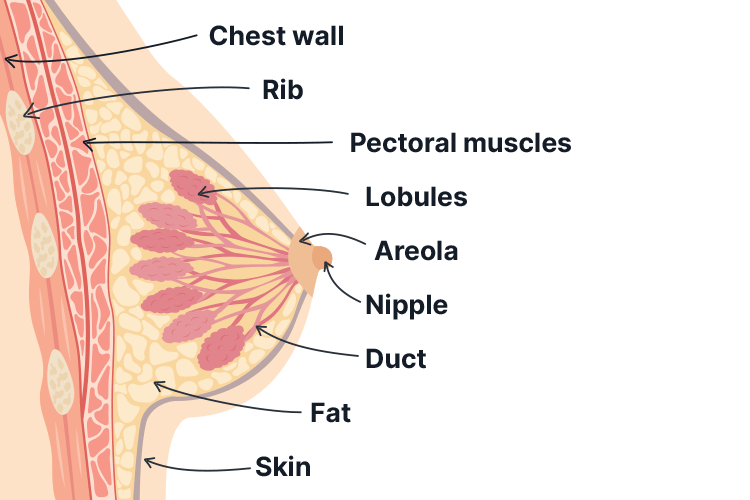
The Breasts
Every person has breast tissue. In people who were assigned female at birth, the breasts comprise lobes, lobules and ducts (Cancer Council Victoria 2022).
Each breast contains between 12 and 20 sections known as lobes. Each one of these lobes contains glands known as lobules that produce milk. Lobes and lobules are connected by thin tubes known as ducts, which carry milk to the nipples (Cancer Council Victoria 2022).
People who were assigned male at birth have ducts, but very few (or even no) lobes and lobules.
Everyone’s breast tissue contains fibrous or fatty tissue (Cancer Council Victoria 2022).
What is Breast Cancer?
Breast cancer occurs when cells that line either the breast ducts or lobules begin to grow abnormally (Cancer Council Victoria 2022).
The exact cause of this abnormal cell growth is not known, but there are identified risk factors (Better Health Channel 2023).
Risk Factors for Breast Cancer
Factors that increase the risk of breast cancer include:
In assigned female at birth people:
- Older age (over 50)
- Having dense breast tissue (as seen on a mammogram)
- Family history of breast cancer or a certain type of ovarian cancer in a first-degree relative (e.g. mother or sister) or in female relatives on the same side of the family (especially if they were diagnosed at a young age)
- Being overweight or gaining weight after menopause
- Excessive alcohol consumption
- Physical inactivity
- Early commencement of menstruation (before the age of 12)
- Giving birth after the age of 30
- Never giving birth
- Never breastfeeding
- Starting menopause after the age of 55
- Certain medicines and treatments:
- Taking menopause hormone therapy (MHT) that contains oestrogen and progestogen
- Taking the contraceptive pill for a prolonged period of time
- Taking diethylstilboestrol (DES) while pregnant
- Undergoing radiation therapy to the chest for Hodgkin lymphoma
- Atypical ductal hyperplasia or proliferative disease without atypia
- Previous diagnosis of lobular carcinoma in situ (LCIS) or ductal carcinoma in situ (DCIS).
In assigned male at birth people, risk factors may include older age, Klinefelter syndrome, and family history (Cancer Council Australia 2022).
(Cancer Council Australia 2022; Better Health Channel 2023)
In assigned male at birth people:
- Older age
- Klinefelter syndrome (a rare genetic disorder where an assigned male at birth person has three sex chromosomes - XXY)
- Family history:
- Having several first-degree relatives who have been diagnosed with BRCA2 breast cancer
- Family history of breast cancer diagnosed under the of 40
- Having several relatives who have been diagnosed with ovarian, colon or prostate cancer.
(Cancer Council Australia 2022)
Signs of Breast Cancer
It’s normal for the breasts to change over time, and while most changes are not caused by cancer, there are some signs that may be indicative of cancer and should be investigated (Better Health Channel 2023). These include:
- A lump, lumpiness or thickening in the breast (particularly if only in one breast)
- Changes in the shape or size of the breast
- Nipple changes (e.g. shape, crusting, sores or ulcers, redness, clear or bloody discharge)
- Inverted nipple
- Skin changes on the breast (e.g. dimpling, indentation, rash, scaliness, redness or changes in colour)
- Swelling or discomfort in the armpit
- Prolonged, unusual pain in one breast only that is unrelated to menstrual cycle symptoms.
(Cancer Council Australia 2022)
Breast Cancer Screening

Under the national BreastScreen Australia program, women aged between 40 and 74 are able to access a free mammogram (breast screen) every two years (DoHaAC 2023).
Screening can detect breast cancer early, even before it’s seen or felt (DoHaAC 2023).
For more information about BreastScreen Australia, see the Department of Health website.
Breast Cancer Diagnosis
Tests to investigate breast changes may include:
- Personal and family history
- Physical examination of the breast and lymph nodes in the armpit and above the collarbone
- Mammogram
- Ultrasound
- Breast MRI
- Biopsy
- Core biopsy - a piece of tissue is removed with a needle
- Vacuum-assisted core biopsy - A larger area of tissue is removed from the breast using a needle attached to a suction instrument
- Fine needle aspiration - a needle is inserted into tissue or a lymph node
- Surgical biopsy performed under general anaesthetic.
(Cancer Council Australia 2022)
If breast cancer is detected, further tests may be conducted to determine whether it has spread. These might include:
- Blood tests
- Bone scan
- CT scan.
(Cancer Council Australia 2022)

Breast Cancer Staging
Breast cancer generally uses the TNM (tumour-nodes-metastasis) staging system (Cancer Council Australia 2022):
- Stage I and II - Early cancer that is contained in the breast. May or may not have spread to lymph nodes in the armpit
- Stage III - The cancer is locally advanced, meaning that it:
- Is larger than 5 cm
- Has spread to nearby tissue (e.g. skin, muscle or ribs), and/or
- Has spread to many lymph nodes
- Stage IV - Advanced and metastatic cancer that has spread to other parts of the body.
(Cancer Council Australia 2022; Healthdirect 2020)
Breast cancer can also be graded to indicate how active the cancer cells are and how quickly they are growing:
- Grade 1 (low): Cancer cells look slightly different to normal cells but are growing slowly
- Grade 2 (intermediate): Cancer cells do not look like normal cells and are growing more quickly than grade 1 cells
- Grade 3 (high): Cancer cells look very different to normal cells and are growing quickly.
(Cancer Council Australia 2022)
Breast Cancer Treatment
The treatment options used will depend on a number of factors, including:
- Patient preferences
- Patient age and general health
- Whether the patient has experienced menopause
- Type of breast cancer
- Size of tumour in relation to the breast
- Stage and grade of the cancer
- Test results.
(Better Health Channel 2023)
Treatment might include a combination of the following:
- Surgical intervention:
- Breast-conserving surgery, where the cancer and surrounding tissue are removed while keeping the rest of the breast intact
- Mastectomy, where the entire breast and armpit lymph nodes are removed (this might be followed by breast reconstruction surgery).
- Radiation therapy
- Chemotherapy
- Hormone therapy
- Palliative care.
(Cancer Council Australia 2022; Better Health Channel 2023; Healthdirect 2020)
Breast Cancer in Trans and Gender-diverse People
Every person has breast tissue (unless it has been removed). This includes men, as well as trans and gender-diverse people (BreastScreen Victoria 2023).
- Trans women (or gender-diverse people who were assigned male at birth) who have been receiving gender-affirming hormones (e.g. oestrogen) for more than five years may be at increased risk of breast cancer and should be screened every two years.
- Trans men (or gender-diverse people who were assigned female at birth) who have not undergone subcutaneous mastectomy (top surgery) are recommended to undergo screening every two years. Trans men who have undergone top surgery are encouraged to consult with their general practitioner about their individual risk factors.
(Cancer Council Victoria 2022; BreastScreen Victoria 2022; Mayo Clinic 2022)
It’s important to note that trans and gender-diverse people are underscreened for breast cancer due to a variety of barriers that deter them from accessing this care. These barriers include:
- Ignorance from staff
- Transphobia
- Fear of being misgendered or needing to ‘out’ themselves
- Lack of awareness about screening
- Embarrassment
- Fear of experiencing gender dysphoria or anxiety due to the test.
(BreastScreen Victoria 2022)
Therefore, it’s important to ensure that breast cancer screening and care is inclusive, welcoming and safe for all patients (BreastScreen Victoria 2022).
For more information on providing LGBT-inclusive practice in healthcare, see the Victorian Department of Health’s resources.
Test Your Knowledge
Question 1 of 3
True or false: It’s abnormal for the breasts to change over time.
Topics
References
- Better Health Channel 2023, Breast Cancer, Victoria State Government, viewed 13 February 2024, https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/breast-cancer
- BreastScreen Victoria 2022, Trans and Gender Diverse People, BreastScreen Victoria, viewed 13 February 2024, https://www.breastscreen.org.au/community-support/trans-and-gender-diverse-people/
- Cancer Council Australia 2022, Understanding Breast Cancer, Cancer Council, viewed 13 February 2024, https://www.cancer.org.au/assets/pdf/understanding-breast-cancer-booklet
- Cancer Council Victoria 2022, Breast Cancer, Cancer Council Victoria, viewed 13 February 2024, https://www.cancervic.org.au/cancer-information/types-of-cancer/breast_cancer/breast-cancer.html
- Department of Health and Aged Care 2023, About the BreastScreen Australia Program, Australian Government, viewed 13 February 2024, https://www.health.gov.au/initiatives-and-programs/breastscreen-australia-program/about-the-breastscreen-australia-program
- Healthdirect 2020, Breast Cancer, Australian Government, viewed 13 February 2024, https://www.healthdirect.gov.au/breast-cancer
- Mayo Clinic 2022, Masculinizing Surgery, Mayo Clinic, viewed 13 February 2024, https://www.mayoclinic.org/tests-procedures/top-surgery-for-transgender-men/about/pac-20469462
 New
New