What is Otitis Media?
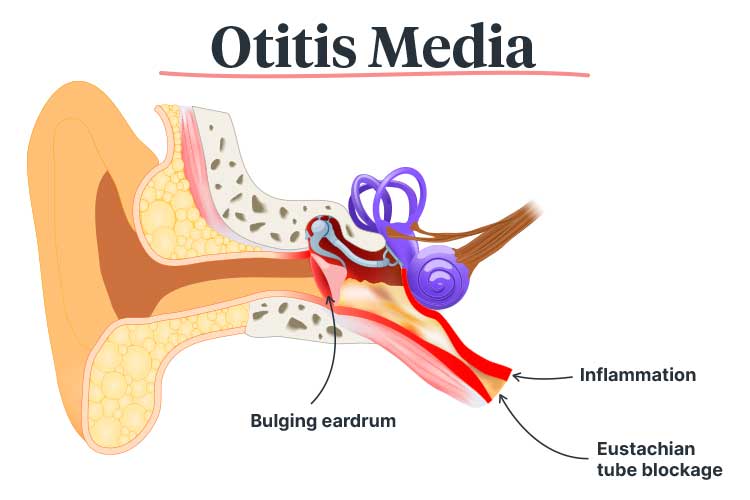
Otitis media is an umbrella term encompassing all types of inflammation and infection of the middle ear, which is the air-filled cavity located behind the eardrum (Children’s Health Queensland 2024; Mayo Clinic 2025).
Otitis media can affect people of all ages, but it is most common among young children, especially those between 6 and 18 months of age. It is estimated that about 75% of children will have experienced at least one episode of otitis media by the time they start school (Healthdirect 2024; RCHM 2021).
In most cases, otitis media arises from a viral or bacterial infection that initially presents as a cold. The infection may then spread to the middle ear through the eustachian tube, causing swelling and a build-up of fluid. As this places pressure on the eardrum, there is a risk that the eardrum will perforate (burst) (Children’s Health Queensland 2024; Danishyar & Ashurst 2023).
Risk Factors for Otitis Media in Children
Children who are at increased risk of otitis media include:
- Aboriginal and Torres Strait Islander children
- Children of low socio-economic status
- Immunocompromised children
- Children who attend daycare
- Children who use a dummy
- Children who are exposed to cigarette smoke.
(RCHM 2021; Danishyar & Ashurst 2023)
Symptoms of Otitis Media
Generally, initial symptoms will be those of a cold, including a sore throat, runny nose and fever. When the infection spreads to the ear, symptoms may include:
- Ear pain
- Headache
- Fever
- Impaired hearing
- Crying
- Pulling or rubbing at the ears
- Irritability
- Loss of appetite
- Fluid or blood drainage from the ear (if the eardrum has perforated).
(Healthdirect 2024; Children’s Health Queensland 2024)
Types of Otitis Media
The main presentations of otitis media are:
Acute Otitis Media

Acute otitis media (AOM) is a painful infection of the middle ear, often with a sudden onset. It may be accompanied by fever, fluid in the middle ear, irritability and a red eardrum bulging with pus (ACSQHC 2021).
AOM is one of the most common causes of severe pain in children, with almost every person experiencing at least one episode during their childhood (ACSQHC 2021; Heathdirect 2024).
Otitis Media With Effusion

Otitis media with effusion (OME), which is also known as glue ear, is characterised by a build-up of fluid in the middle ear (ACSQHC 2021).
OME is not an acute infection. It often occurs when fluid accumulates in the middle ear and eustachian tube following a cold or episode of AOM. Generally, the only symptom of OME is hearing impairment due to the fluid obstruction (Searight et al. 2023). The condition is not painful but may cause annoyance. As the signs of OME are subtle, it is easy to overlook (ACSQHC 2021).
Most episodes of OME resolve on their own within three months. However, 25% of children will experience ongoing OME and consequently persistent hearing interference. This may lead to difficulties with language, education and behaviour (ACSQHC 2021).
A child with OME may display the following behaviours:
- Rubbing or pulling their ears
- Lack of attention
- Speech delays or changes
- Turning music or the television volume up
- Not ‘listening’
- Difficulties with balance.
(SCHN 2024)
Chronic Suppurative Otitis Media

Chronic suppurative otitis media (CSOM), also known as runny ear, describes chronic (for two and six weeks) drainage of ear discharge through a perforation (hole) in the eardrum (i.e. tympanic membrane) (ACSQHC 2021; Rosario & Mendez 2023).
CSOM may arise as a complication of AOM if the pressure caused by swelling and fluid perforates the eardrum. Other potential causes include eustachian tube obstruction, ear injuries and blast injuries (Jan 2024).
Discharge will drain profusely and may range from yellow to clear. In most cases, it is not painful or accompanied by inflammation, but may have a foul smell (Jan 2024; Varughese 2023).
CSOM is the most disabling type of otitis media and is difficult to treat. Drainage may continue for years and may even lead to permanent hearing loss (ACSQHC 2021).
Treatment of Otitis Media
Treatment of acute otitis media generally involves symptom management using analgesics. Bacterial infections may be treated with antibiotics (Children’s Health Queensland 2024).
CSOM typically requires manual removal of drainage and topical antibiotics (Tidy 2023).
In most cases, otitis media will resolve on its own (ACSQHC 2021).
Otitis Media in Aboriginal and Torres Strait Islander Children
Otitis media is a significant issue affecting Aboriginal and Torres Strait Islander children, who have the highest rate of middle ear disease in the world. They are also more likely to experience earlier, more severe and longer-lasting middle ear disease than non-Indigenous children (ACSQHC 2021).
In fact, a report published in the Medical Journal of Australia in 2021 found that in remote Northern Territory communities, only 1 in 10 Aboriginal children under the age of three had healthy ears, while 5 in 10 had OME and 4 in 10 had CSOM (Leach et al. 2021).
The rate, frequency and severity of otitis media in Aboriginal and Torres Strait Islander children are comparable to that of children living in developing countries (DeLacy et al. 2020).
Aboriginal and Torres Strait Islander children who experience hearing loss within their first 1,000 days of life are at risk of delayed speech and language development, which may lead to issues that carry into adulthood (ACSQHC 2021). These include:
- Education difficulties
- Impaired language development and speech issues
- Vulnerability upon starting school
- Inattention
- Non-attendance at school
- Early school leaving
- Social isolation
- Reduced education and employment opportunities.
(ACSQHC 2021; Leach et al. 2021)
Risk Factors for Otitis Media in Aboriginal and Torres Strait Islander Children
The prevalence of otitis media in Aboriginal and Torres Strait Islander communities is associated with social determinants of health and environmental factors, including:
- Overcrowded housing, which has been identified as the most significant risk factor for ‘upper respiratory tract carriage’
- Poor housing conditions
- Exposure to cigarette smoke
- Socioeconomic disadvantage
- Poverty and low income
- Difficulty accessing health services
- Poor hygiene
- Lack of education
- Unemployment and lack of employment opportunities
- Malnutrition
- Lack of community involvement in service provision and planning
- Cultural and language differences
- Premature birth
- Being bottle-fed, especially ‘prop feeding’ wherein the bottle is propped up so that the infant can feed without supervision, or if the infant falls asleep with a bottle in their mouth.
(DeLacy et al. 2020; NSW Health 2024)
What is Myringotomy?
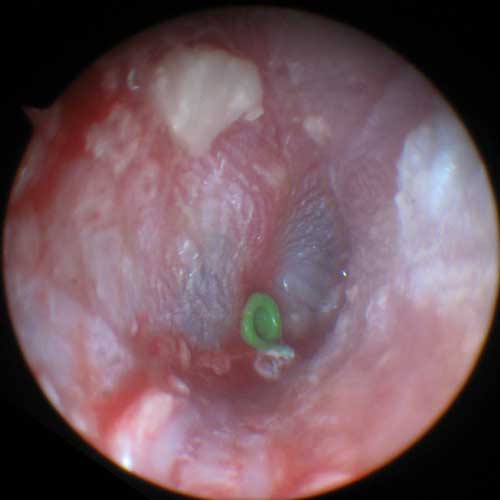
Myringotomy is a surgical procedure used to treat otitis media wherein a small incision is made in the eardrum in order to drain discharge from the middle ear. Grommets (tympanostomy tubes) are often inserted to ensure the incision stays open, facilitating ventilation and drainage (ACSQHC 2021).
What are the Benefits of Myringotomy?
While myringotomy is generally not a first-line treatment for AOM or OME, it may be beneficial in some situations. Clinical practice guidelines recommend myringotomy for children who have been experiencing OME in both ears for longer than three months and have documented hearing loss. The more severe the hearing loss, the more likely myringotomy is to be beneficial to the child (ACSQHC 2021).
Furthermore, myringotomy is potentially effective in reducing recurrent ASOM episodes, however, more evidence is needed. Clinical practice guidelines in the United States recommend the procedure for children who have experienced:
- Three episodes of AOM in six months, or
- Four episodes of AOM in one year.
(ACSQHC 2021a)
Generally, grommets should only be inserted if OME is also present. Whether grommets are more effective than antibiotics in reducing recurrent AOM is still uncertain (ACSQHC 2021).
Potential Complications of Myringotomy
- Discharge through the grommets, which affects about 25% of children
- Eardrum perforation.
(ACSQHC 2021)
Myringotomy in Australia
Myringotomy with grommet insertion is one of the most common paediatric surgical procedures in Australia, especially for those aged between 0 and 4 years of age (ACSQHC 2021).
Despite this, according to the Fourth Australian Atlas of Healthcare Variation, Aboriginal and Torres Strait Islander children receive less myringotomy than what is expected based on the prevalence of otitis media in Aboriginal and Torres Strait Islander communities (ACSQHC 2021).
This suggests that:
- Some Aboriginal and Torres Strait Islander children who would benefit from myringotomy do not receive it
- Some non-Aboriginal or Torres Strait Islander children are undergoing myringotomy despite not needing it.
(ACSQHC 2021)
How Can Otitis Media Care in Aboriginal and Torres Strait Islander Children be Improved?

According to the Atlas, a ‘comprehensive approach’ is required in order to improve the prevention, diagnosis and treatment of otitis media in Aboriginal and Torres Strait Islander children (ACSQHC 2021).
One important consideration is Aboriginal and Torres Strait Islander communities’ holistic approach towards health, which includes ‘body, mind, spirit, land, environment, custom, socioeconomic status, family and community’ and differs from the ‘mainstream’ approach (DeLacy et al. 2020).
Strategies that may help to reduce the prevalence of otitis media in Aboriginal and Torres Strait Islander communities include:
- Encouraging breastfeeding rather than bottle-feeding
- Ensuring children get adequate nutrition
- Ensuring children have safe and healthy housing conditions
- Ensuring children are up-to-date with their immunisation schedule
- Medical services providing patient and community education, screening and smoking cessation advice in a culturally appropriate way
- Newborn hearing screening.
(NSW Health 2024; Liotta 2018)
Furthermore, strategies should be put into place to ensure that Aboriginal and Torres Strait Islander children who require myringotomy are able to receive it. These include:
- Improving the monitoring of ear health
- Improving training in the diagnosis of middle ear disease
- Updating relevant guidelines
- Improving Aboriginal and Torres Strait Islander peoples’ ability to access hearing support services and audiologists
- Improving Aboriginal and Torres Strait Islander peoples’ ability to access ear, nose and throat specialists
- Empowering shared decision-making
- Improving the collection of data.
(ACSQHC 2021)
Test Your Knowledge
Question 1 of 3
What percentage of children have experienced at least one episode of otitis media by the time they start school?
Topics
References
- Australian Commission on Safety and Quality in Health Care 2021, Fourth Australian Atlas of Healthcare Variation 2021, Australian Government, viewed 12 May 2025, https://www.safetyandquality.gov.au/publications-and-resources/resource-library/fourth-australian-atlas-healthcare-variation-2021
- Children’s Health Queensland Hospital and Health Service 2024, Middle Ear Infection (Acute Otitis Media), Queensland Government, viewed 12 May 2025, https://www.childrens.health.qld.gov.au/fact-sheet-middle-ear-disease/
- Danishyar, A & Ashurst, JV 2023, ‘Acute Otitis Media’, StatPearls, viewed 12 May 2025, https://www.ncbi.nlm.nih.gov/books/NBK470332/
- DeLacy, J, Dune, T & Macdonald, JJ 2020, ‘The Social Determinants of Otitis Media in Aboriginal Children in Australia: Are We Addressing the Primary Causes? A Systematic Content Review’, BMC Public Health, viewed 12 May 2025, https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-020-08570-3
- Healthdirect 2024, Otitis Media (Middle Ear Infection), Australian Government, viewed 12 May 2025, https://www.healthdirect.gov.au/otitis-media
- Jan, TA 2024, Otitis Media (Chronic Suppurative), MSD Manual, viewed 12 May 2025, https://www.msdmanuals.com/en-au/home/ear,-nose,-and-throat-disorders/middle-ear-disorders/otitis-media-chronic-suppurative
- Leach, AJ, Morris, PS, Coates, HLC et al. 2021, ‘Otitis Media Guidelines for Australian Aboriginal and Torres Strait Islander Children: Summary of Recommendations’, Medical Journal of Australia, vol. 214, no. 5, viewed 12 May 2025, https://onlinelibrary.wiley.com/doi/10.5694/mja2.50953
- Liotta, M 2018, ‘Targeting Hearing Loss in Aboriginal and Torres Strait Islander Communities’, NewsGP, viewed 12 May 2025, https://www1.racgp.org.au/newsgp/racgp/targeting-hearing-loss-in-aboriginal-and-torres-st
- Mayo Clinic 2025, Ear Infection (Middle Ear), Mayo Clinic, viewed 12 May 2025, https://www.mayoclinic.org/diseases-conditions/ear-infections/symptoms-causes/syc-20351616
- NSW Health 2024, NSW Aboriginal Ear Health Program, New South Wales Government, viewed 12 May 2025, https://www.health.nsw.gov.au/kidsfamilies/MCFhealth/Pages/aboriginal-ear-health.aspx
- Rosario, DC & Mendez, MD 2023, ‘Chronic Suppurative Otitis’, StatPearls, viewed 12 May 2025, https://www.ncbi.nlm.nih.gov/books/NBK554592/
- The Royal Children's Hospital Melbourne 2021, Acute Otitis Media, RCHM, viewed 12 May 2025, https://www.rch.org.au/clinicalguide/guideline_index/Acute_Otitis_Media/
- Searight, FT, Singh, R & Peterson, DC 2023, ‘Otitis Media With Effusion’, StatPearls, viewed 12 May 2025, https://www.ncbi.nlm.nih.gov/books/NBK538293/
- The Sydney Children’s Hospital Network 2024, Ear Infections and Glue Ear, New South Wales Government, viewed 12 May 2025, https://www.schn.health.nsw.gov.au/ear-infections-and-glue-ear-factsheet
- Tidy, C 2023, Chronic Suppurative Otitis Media, Patient, viewed 12 May 2025, https://patient.info/doctor/chronic-suppurative-otitis-media
- Varughese, D 2023, Chronic Suppurative Otitis Media Clinical Presentation, Medscape, viewed 12 May 2025, https://emedicine.medscape.com/article/859501-overview
 New
New 
