Traumatic spinal cord injury (SCI) is a very serious presentation with the potential to cause significant, lifelong disability (Bennett et al. 2024). There are currently about 20,800 people in Australia living with an SCI (AlphaBeta Australia 2020).
In cases of suspected SCI, immediate, appropriate management is crucial in preventing further trauma and maintaining the physiological stability of the patient (RCHM 2023).
What is the Spinal Cord?
The spinal cord, which together with the brain comprises the central nervous system, is a column of nerve tissue responsible for several critical functions, including the transmission of motor and sensory signals between the brain and peripheral nervous system and the control of certain reflexes (QBI 2022).
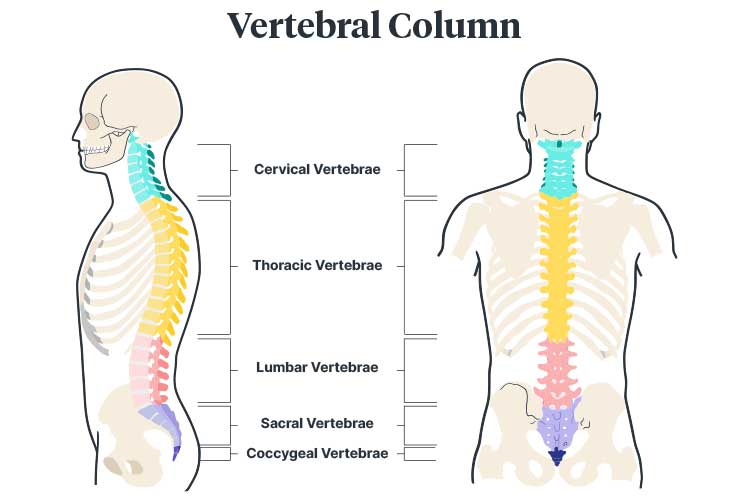
The spinal cord extends downwards from the brainstem and is protected by 26 bones known as vertebrae, which are collectively called the vertebral column (QBI 2022). The vertebral column is split into five sections:
- Cervical spine (C1-C7) in the neck
- Thoracic spine (T1-T12) in the mid-back
- Lumbar spine (L1-L5) in the lower back
- Sacrum
- Coccyx.
(Hines 2018)
What is a Spinal Cord Injury?
A spinal cord injury (SCI) occurs when the spinal cord is damaged via compression (axial loading), bruising, hyperflexion, hyperextension, rotation or penetration, causing loss of feeling or functional mobility (SCIA 2023a; QAS 2020).
In most cases of SCI, the spinal cord is still physically intact despite being damaged (SCIA 2023a). It is also possible for the spinal cord to be damaged in the absence of vertebral injury, known as spinal cord injury without radiographic abnormality (SCIWORA) (Campos 2024).
Vertebrae can also be fractured without damaging the spinal cord itself, but this is not an SCI (SCIA 2023a).
Essentially, an SCI damages the connection between the brain and the body systems responsible for sensory, motor and autonomic function below the site of the injury (AANS 2024).
Patients with an SCI may experience a complete or partial loss of sensory and/or motor function in their arms, legs and/or body. The extent of symptoms depends on the severity of the injury and the area of the spinal cord that was damaged. In serious cases, SCI may affect continence, breathing, heart rate and blood pressure (WHO 2024).
An SCI can be either complete or incomplete:
- A complete SCI is when there is a total loss of motor and sensory function below the level of the injury (i.e. no movement or feeling)
- An incomplete SCI is when there is still some motor and, or sensory function below the level of the injury (i.e. some movement and, or feeling).
(AANS 2024; Mayo Clinic 2024)
Furthermore, the paralysis caused by SCI can be described as:
- Paraplegia - loss of motor and sensory function in the legs, pelvic organs and part or all of the trunk
- Tetraplegia/quadriplegia - loss of motor and sensory function in the legs, pelvic organs, trunk, arms and hands (to varying degrees and determined by the level of injury in the spinal cord).
(Mayo Clinic 2024)
Causes of Spinal Cord Injury
SCIs have either traumatic or non-traumatic (e.g. tumour, degenerative disorder) causes (AlphaBeta Australia 2020).
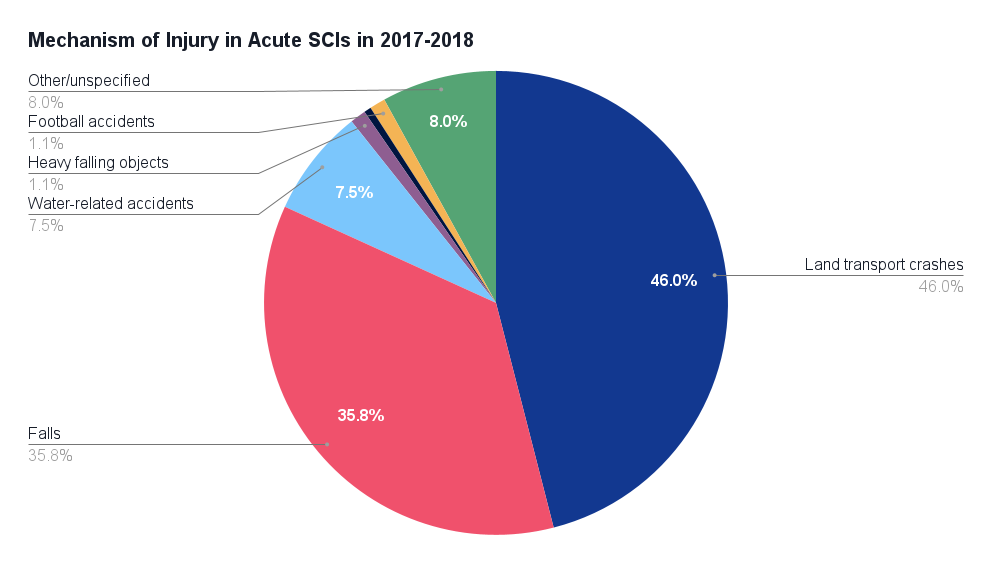
In 2017-2018, the most common causes of traumatic SCI included:
- Land transport crashes (46%), involving motor vehicle occupants (17.1%) and unprotected land transport users such as motorcyclists (28.9%)
- Falls (35.8%), including falls from heights of over 1 metre (21.4%) and falls from under 1 metre or the same level (14.4%)
- Water-related accidents, such as diving into shallow water or surfing accidents (7.5%)
- Trauma from heavy falling objects (1.1%)
- Horse-related accidents (0.5%)
- Football accidents (1.1%).
(AIHW 2021)
Overall, 60% of all SCIs are traumatic, while 40% are non-traumatic (AlphaBeta Australia 2020).
About 23% of injuries between 2017-2018 were sustained during sports or leisure activities, while 11% were sustained while working for income (AIHW 2021).
Interestingly, traumatic SCIs are much more common in people aged under 65 (accounting for 81% of SCIs in that age group) but less common in those over 65 (comprising only 29% of cases) (AlphaBeta Australia 2020). This is likely due to changes in physical habits as people age.
In 2017-2018, 80% of those who experienced an SCI were male, and the most affected age group was 25 to 34-year-olds (accounting for 21% of cases) (SCIA 2023b).
Symptoms of Acute Spinal Cord Injury
An SCI should be suspected in:
- Any unconscious trauma patient
- A patient who has sustained a mechanism of injury that might impact the spinal cord, including injury to the head
- A patient complaining of spinal pain or neurological symptoms (noting that a distracting injury such as a painful limb may prevent the patient from adequately identifying spinal pain).
Depending on the specifics of the injury, a patient who has experienced an SCI may acutely present with:
- Flaccidity and paralysis below the level of injury (in the arms, chest and/or legs)
- Loss of spinal reflexes below the level of injury
- Paraesthesia - altered sensation below the level of injury
- Loss of sweating below the level of injury
- Loss of bowel and bladder function
- Respiratory compromise
- Loss of proprioception (sense of body position)
- Hypotension
- Bradycardia
- Loss of thermoregulation
- Priapism (prolonged penile erection).
(QAS 2020; RCHM 2023; Berlowitz et al. 2016)
Shock Associated With Spinal Injury
Shock in a trauma patient with an SCI must always be considered hypovolaemic (haemorrhagic) until proven otherwise, as the management is different to spinal - neurogenic shock (Singhal & Aggarwal 2016).
There are two types of SCI-related shock:
- Spinal shock, which involves the loss of all sensation below the level of injury, is not circulatory in nature.
- Neurogenic shock is the haemodynamic component of spinal shock, which occurs in injuries above T6. It presents as hypotension, bradycardia and peripheral vasodilation. These serious haemodynamic changes result from a sudden loss of autonomic tone due to the SCI.
(Singhal & Aggarwal 2016; Ziu et al. 2024)
Assessment and Management of an Acute Spinal Injury

General Principles
The goal of pre-hospital management of an acute SCI is to minimise neurological deficit and prevent further injury by:
- Treating the patient as having a high probability of SCI
- Identifying and reversing any immediate threats to life
- Appropriately restricting spinal motion in order to maintain the integrity of the spinal column and, therefore, the cord
- Providing cardiovascular and ventilation support when required
- Maintaining thermoregulation, as neurogenic shock can impair the regulation of body temperature.
(QAS 2020; Ambulance Victoria 2024; Dave et al. 2023)
Management of Acute Spinal Cord Injury
1. Early Activation
Upon initial notification of a suspected SCI, you need to:
- Gather vital information about the patient using the MIST mnemonic:
- M - mechanism of injury
- I - injuries found or suspected
- S - signs (respiratory rate, pulse, blood pressure, oxygen saturation, and neurological state using AVPU)
- T - Treatments already given, if any.
- Don PPE (gloves, aprons and eye protection).
- Activate the trauma team and available support departments.
- Ensure the trauma bay is ready to receive the patient (equipment checks, documentation, medications and resuscitation equipment).
- Assign roles to each member of the responding care team.
(Trauma Victoria 2017)
2. Primary Survey
Note: For a comprehensive explanation of the ABCDE approach, read How To Assess a Deteriorating / Critically Ill Patient (ABCDE Assessment).
Perform a primary survey using the ABCDE approach to manage any life-threatening conditions:
- A - Airway:
- Assess the stability of the airway
- Perform simple airway manoeuvres (chin lift or jaw thrust) to open the airway if required
- Secure the airway if required, ensuring you maintain full spinal precautions.
- B - Breathing:
- Assess ventilation via respiratory rate and perfusion via oxygen saturation
- Perform chest auscultation to check for abnormal breath sounds and assess bilateral air entry
- Observe for diaphragmatic breathing
- Apply oxygen and ventilate if required.
- C - Circulation:
- Gain intravenous access
- Administer fluids if there is evidence of life-threatening bleeding and shock. Hypotension should be avoided
- Apply direct pressure to any external bleeding
- D - Disability:
- Check the level of consciousness using an initial AVPU assessment
- Check blood glucose levels
- Combative patients should not be restrained to reduce the risk of further injury. They may need to be sedated, intubated and ventilated (note, however, that this would be a difficult intubation due to the inability to move the patient’s neck).
- E - Exposure/environment:
- Fully remove the patient’s clothing
- Maintain thermoregulation.
- Log roll the patient, palpate the spinal column and assess anal tone.
(Trauma Victoria 2017)
3. Secondary Survey
Note: A secondary survey must only be performed after a primary survey has been completed and after any life-threatening injuries have been managed.
- Obtain patient history from the patient and/or emergency personnel in order to gain a better understanding of the injury. Use the AMPLE acronym to obtain all the necessary information:
- A - allergies
- M - medication
- P - past medical history (including tetanus status)
- L - last meal
- E - events leading to the injury (bystanders may be able to assist with this).
- Perform a thorough head-to-toe examination, assessing the patient’s motor, sensory and reflex capacity.
(Trauma Victoria 2017)
4. Early Management
- If there is a potential for airway deterioration, consider intubation.
- Treat hypovolaemia with fluid as per local policy. Avoid fluid overload if the patient is suspected of experiencing neurogenic shock. Monitor fluid balance.
- Monitor heart rate, respiration rate, blood pressure and oxygen saturation every 15 minutes.
- Administer analgesia (typically morphine or fentanyl) and consider administering anti-emetics.
- Prevent hypothermia by covering the patient with warm blankets and using a forced air-warming machine.
- Perform a detailed neurological assessment using the Glasgow Coma Scale (GCS).
- Perform pathology tests for FBC (full blood count), UEC (urea electrolytes and creatinine), glucose and blood gases.
- Perform wound care.
- Perform pressure area care.
- Insert an indwelling urinary catheter and measure urine output hourly.
- Keep the patient nil-by-mouth in the initial post-resuscitation stage. Consider inserting a nasogastric tube.
- Reassess the patient frequently to identify deterioration. Repeat ABCDE if required.
(Trauma Victoria 2017)
Other Considerations
Immobilisation Techniques
Immobilisation techniques are used in cases of suspected SCI to ‘support the neutral alignment of the spinal column and reduce or distribute forces placed on it’ (Ambulance Victoria 2024).
Typically, this involves the use of a rigid cervical collar as well as full-length spinal protection (Feller et al. 2022).
However, in recent years, there have been growing concerns about the use of immobilisation techniques, specifically:
- Patient distress and discomfort
- Prolonging the prehospital period and potentially delaying important investigations and treatments
- Interference with other interventions
- Impairment of the patient’s respiration due to being strapped in the supine position, especially in cases of chest trauma
- Increased difficulty of intubation
- In patients with pre-existing spinal deformity, forcing the patient into a predetermined position could potentially cause further harm.
(Feller et al. 2022)
A recent systematic review of literature on immobilisation techniques noted that evidence supporting these practices is ‘sparse’, recommending that:
- Immobilisation should not be used for patients with isolated penetrating trauma, as they may be ABCDE-unstable and require surgical intervention that should not be delayed
- Rigid cervical collars and hard backboards should not be used for ABCDE-stable patients, as there is a risk of secondary traumatic SCI
- ABCDE-stable patients with a neurologic deficit and/or osseous pain may be stabilised using a vacuum mattress.
(Maschmann et al. 2019)
Overall, there is very little evidence demonstrating the efficacy of hard backboards, with studies instead favouring soft surface stretcher systems such as vacuum mattresses (Maschmann et al. 2019).
Remember to always refer to your local policy and best practice procedures on immobilisation techniques.
Spinal Clearance
Spinal clearance is the process of determining the cervical spine stability of a trauma patient to identify any missed cervical spine injuries, which can have severe consequences. After clearance, immobilisation can be ceased (Alfred Health 2009; Nickson 2024).
Your local policy will determine the exact protocol you’re required to follow. This might be based on the Canadian C-Spine Rule, which is a well-validated decision tool that can be used to rule out cervical spine injury without the need for radiographic imaging in trauma patients who are alert and stable (MDCalc 2022).
Spinal clearance has become a highly controversial topic (Alfred Health 2009) because it can be achieved clinically and/or radiologically. For more information, we recommend reviewing more resources. Nickson (2024) offers a practical approach to determining the best course of action.
Always follow your local policies and procedures on spinal clearance.
Conclusion

Spinal cord injury is rare but potentially devastating for patients and may cause significant disability, reduced quality of life and decreased ability to work and participate in the community (Berlowitz et al. 2016).
Management of an acute SCI is time-critical and requires great care to reduce the risk of further injury to the patient.
Always refer to your local policies and procedures.
Test Your Knowledge
Question 1 of 3
Which type of SCI-induced shock is circulatory in nature?
Topics
Further your knowledge
References
- Alfred Health 2009, The Alfred Spinal Clearance Management Protocol, Alfred Health, viewed 19 September 2024, https://www.alfredhealth.org.au/images/resources/clinical-resources/SpinalClearanceManagementProtocol_External.pdf
- AlphaBeta Australia 2020, Spinal Cord Injury in Australia: The Case For Investing in New Treatments, AlphaBeta Australia, viewed 19 September 2024, https://treasury.gov.au/sites/default/files/2021-05/171663_the_australian_spinal_cord_injury_research_collaborative_supporting_document_3.pdf
- Ambulance Victoria 2024, Clinical Practice Guidelines Ambulance and MICA Paramedics, Ambulance Victoria, viewed 20 September 2024, https://www.ambulance.vic.gov.au/wp-content/uploads/2018/11/Clinical-Practice-Guidelines-2018-Edition-1.5.pdf
- American Association of Neurological Surgeons 2024, Spinal Cord Injury, AANS, viewed 19 September 2024, https://www.aans.org/en/Patients/Neurosurgical-Conditions-and-Treatments/Spinal-Cord-Injury
- Australian Institute of Health and Welfare and Flinders University 2021, Spinal Cord Injury, Australia 2017–18, Australian Government, viewed 19 September 2024, https://www.aihw.gov.au/getmedia/5b4a8579-a010-40f0-9ad6-31522a4fcc12/aihw-injcat-219.pdf.aspx?inline=true
- Bennett, J, Das, JM & Emmady, PD 2024, ‘Spinal Cord Injuries’, StatPearls, viewed 19 September 2024, https://www.ncbi.nlm.nih.gov/books/NBK560721/
- Berlowitz, DJ, Wadsworth, B & Ross, J 2016, ‘Respiratory Problems and Management in People With Spinal Cord Injury’, Breathe (Sheff)., vol. 12, no. 4, viewed 20 September 2024, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5335574/
- Campos, A 2024, SCIWORA, Radiopaedia, viewed 19 September 2024, https://radiopaedia.org/articles/sciwora
- Dave, S & Dahlstrom, JJ & Weisbrod, LJ 2023, ‘Neurogenic Shock’, StatPearls, viewed 20 September 2024, https://www.ncbi.nlm.nih.gov/books/NBK459361/
- Feller, R, Furin, M, Alloish, A & Reynolds, C 2022, ‘EMS Immobilization Techniques’, StatPearls, viewed 20 September 2024, https://www.ncbi.nlm.nih.gov/books/NBK459341/
- Hines, T 2018, Anatomy of the Spine, Mayfield Brain & Spine, viewed 19 September 2024, https://www.spineuniverse.com/anatomy
- Maschmann, C, Jeppesen, E, Rubin, MA & Barfod, C 2019, ‘New Clinical Guidelines on the Spinal Stabilisation of Adult Trauma Patients – Consensus and Evidence Based’, Scandinavian Journal of Trauma, Resuscitation and Emergency Medicine, vol. 27, no. 77, viewed 19 September 2024, https://sjtrem.biomedcentral.com/articles/10.1186/s13049-019-0655-x
- Mayo Clinic 2024, Spinal Cord Injury, Mayo Clinic, viewed 19 September 2024, https://www.mayoclinic.org/diseases-conditions/spinal-cord-injury/symptoms-causes/syc-20377890
- MDCalc 2022, Canadian C-Spine Rule, MDCalc, viewed 20 September 2024, https://www.mdcalc.com/canadian-c-spine-rule
- Nickson, C 2024, Cervical Spine Assessment, Life in the Fast Lane, viewed 19 September 2024, https://litfl.com/cervical-spine-assessment/
- Queensland Ambulance Service 2020, Clinical Practice Guidelines: Trauma/Spinal Cord Injury, Queensland Government, viewed 19 September 2024, https://www.ambulance.qld.gov.au/__data/assets/pdf_file/0022/219145/cpg_spinal-cord-injury.pdf
- Queensland Brain Institute 2022, The Spinal Cord, The University of Queensland, viewed 19 September 2024, https://qbi.uq.edu.au/brain/brain-anatomy/spinal-cord
- The Royal Children's Hospital Melbourne 2023, Spinal Cord Injury (Acute Management), RCHM, viewed 19 September 2024, https://www.rch.org.au/rchcpg/hospital_clinical_guideline_index/Spinal_Cord_Injury_Acute_Management/
- Singhal, V & Aggarwal, R 2016, ‘Chapter 11 - Spinal Shock’, in H Prabhakar (ed.), Complications in Neuroanesthesia, viewed 20 September 2024, https://www.sciencedirect.com/science/article/pii/B9780128040751000110
- Spinal Cord Injuries Australia 2023b, Spinal Cord Injury Statistics in Australia, SCIA, viewed 19 September 2024, https://scia.org.au/sci-statistics/
- Spinal Cord Injuries Australia 2023a, What is a Spinal Cord Injury?, SCIA, viewed 19 September 2024, https://scia.org.au/what-is-a-spinal-cord-injury/
- Trauma Victoria 2017, Spinal Trauma Guideline, Victoria State Government, viewed 20 September 2024, https://trauma.reach.vic.gov.au/resources/trauma-victoria-guideline-pdf
- World Health Organisation 2024, Spinal Cord Injury, WHO, viewed 19 September 2024, https://www.who.int/news-room/fact-sheets/detail/spinal-cord-injury
- Ziu, E, Weisbrod, LJ & Mesfin, FB 2024, ‘Spinal Shock’, StatPearls, viewed 20 September 2024, https://www.ncbi.nlm.nih.gov/books/NBK448163/
 New
New 

