Syringe drivers help to improve the comfort of patients receiving palliative care. However, they may cause serious harm if healthcare professionals are unfamiliar with the associated equipment and procedures (CareSearch 2021).
Knowing how these devices work and being able to appropriately operate and care for them is crucial in ensuring patients’ safety.
Note: ‘Syringe driver’ is a general term used to describe subcutaneous infusion devices, but you may come across specific brand names.
What Are Syringe Drivers?
Syringe drivers are used to deliver medicines to people who are receiving palliative care when other routes of administration are deemed inappropriate or ineffective for the patient (palliAGED 2021).
The devices themselves are small, portable, battery-operated pumps used to inject medicines subcutaneously (i.e. under the skin). They administer medicines at a continuous rate, usually over a 24-hour period (although the device can stay in situ for up to 14 days) (BSPCC 2020; palliAGED 2021).
Syringe drivers eliminate the need for repeated doses of medicine to be delivered and allow two or three medicines to be administered concurrently (as long as the medicine combinations are compatible) (palliAGED 2021).
When used in community settings, they also help to ensure medicines are taken consistently and reduce the burden placed on family members and carers who would otherwise administer the medicines themselves (CareSearch 2021).

What Are Syringe Drivers Used For?
Patients who are in the final stages of their lives may experience distressing symptoms such as:
- Nausea
- Vomiting
- Pain
- Difficult or noisy breathing
- Excessive secretions
- Fatigue
- Agitation
- Delirium.
(Queensland Health 2018; palliAGED 2021)
Ensuring that these patients are kept as comfortable as possible - which includes alleviating their symptoms with medication - is an essential part of palliative care. However, the physiological changes associated with the dying process may make it more difficult to administer medicines orally (palliAGED 2021).
Oral administration is the preferred route, but it isn’t always feasible. Furthermore, other routes of administration (e.g. intravenous, intramuscular, suppositories) are more invasive and may result in infection. In these cases, syringe drivers are preferred (palliAGED 2021).
In some cases, the syringe driver will only need to be used temporarily, and the patient can go back to oral medicines (e.g. if nausea and vomiting are controlled and there are no other issues) (BPAC NZ 2012).
Indications for Using a Syringe Driver
Patients who should receive subcutaneous infusion via syringe driver are those experiencing:
- Swallowing difficulties due to dysphagia or a physical obstruction (e.g. tumour) in the mouth, throat or oesophagus (i.e. inability to swallow oral medicines)
- Altered level of consciousness
- Weakness
- Nausea and vomiting (i.e. difficulty keeping oral medicines down)
- Poor enteral absorption of medicines
- Severe constipation or faecal impaction.
(SESLHD 2022; palliAGED 2021; Queensland Health 2018)
Contraindications for Using a Syringe Driver
On the other hand, syringe drivers should not be used if:
- There are other viable administration routes available
- There are any contraindications related to the specific medicines being administered
- The patient and/or their family carer have not given consent.
(Queensland Health 2018)
Benefits and Limitations of Syringe Drivers
| Benefits | Limitations |
|---|---|
| Compatible medicines can be administered concurrently, allowing multiple symptoms to be managed at the same time | Potential for technical problems such as flat batteries, kinks in the tubing etc. |
| Allows medicines to bypass the gut | Skin irritation may occur at the insertion site |
| Avoids the ‘peaks and troughs’ of intermittent doses, which provides more consistent symptom control | Might be inappropriate for highly agitated patients |
| Versatile, convenient and accessible | Patients may find the syringe driver bothersome (e.g. restricting clothing choices, causing difficulty bathing, being noisy, interfering with sleeping positions etc.) |
| Ambulant patients can continue performing daily activities while the device is in situ | Patients may find the syringe driver disconcerting or an indicator of ‘impending death’ |
| Removes the need for frequent injections or oral dosages | Requires medicines to be anticipated 24 hours in advance |
| More comfortable and less invasive than other routes of administration (e.g. intramuscular and intravenous) | Other administration routes may still need to be used (e.g. until symptoms are being adequately controlled by the syringe driver or if the patient is experiencing breakthrough symptoms) |
| Allows patients to stay at home with their families. |
(palliAGED 2021; Queensland Health 2018, 2020a; BPAC NZ 2012)
Insertion Sites
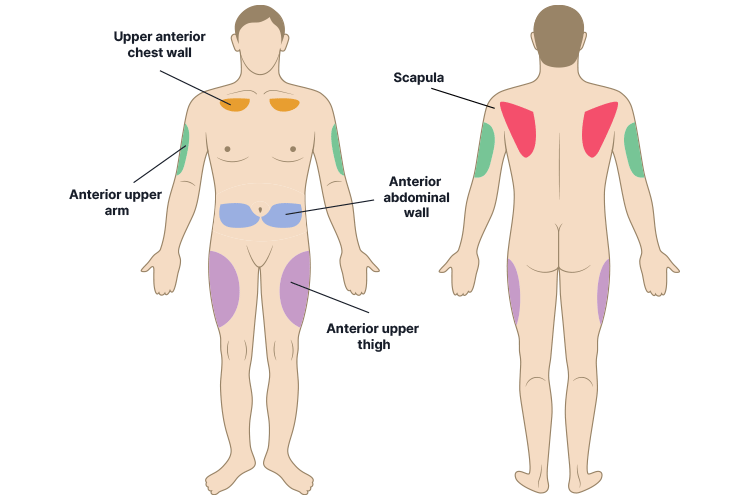
As a general rule, the syringe driver should be inserted into an area of the body that:
- Has a sufficient depth of subcutaneous fat
- Is not near a joint
- Is easily accessible.
(Queensland Health 2021)
Other factors that should be taken into consideration include:
- The patient’s mobility
- The patient’s anxiety and stress levels
- The patient’s preference if they have one
- Pressure care needs.
(Queensland Health 2021; BSPCC 2020)
The preferred sites are the abdomen or anterior chest wall. However, the scapula is more suitable for agitated or distressed patients who may try to dislodge the device. The anterior upper arm or anterior upper thigh are also viable choices if the patient is ambulatory. The abdomen is best for cachectic patients (Queensland Health 2021).
Insertion sites vary in longevity but can be used for up to 14 days, depending on the size of the cannula and the medicines being administered. Sites should be rotated to protect skin integrity and routinely checked for irritation or complications (Queensland Health 2021).
Inappropriate sites include:
- Infected, broken, inflamed or bruised skin
- Areas near or over joints or bony prominences
- Skin folds or breast tissue
- Scarring
- Areas that have recently been irradiated
- Areas of ascites or pitting oedema
- Areas of lymphoedema or compromised lymphatic drainage (e.g. mastectomy sites)
- Tumour sites.
(Queensland Health 2021; BSPCC 2020)
These sites will either impair absorption, increase the risk of infection, cause discomfort or prevent the device from being properly secured (NMHS 2021).
Using Syringe Drivers
The exact procedures for cannulation, medicine administration, maintenance and cannula removal will depend on the specific model of syringe driver being used. For further advice, read the instruction manual of your device and refer to your local policies and procedures.
For in-depth guidance, see Queensland Health’s Guidelines for Subcutaneous Infusion Device Management in Palliative Care and Other Settings.
General Guidelines
- Always provide the patient and their family with a full explanation of the device and gain their informed consent prior to cannulation.
- Use aseptic technique when changing and re-cannulating.
- Assess the insertion site at least every four hours. Ask the patient how they feel and whether their symptoms are being controlled, ensure the device is working, check the volume of the syringe relative to the time, check the patency of the tubing and ensure all connections are firm with no leakages.
- Only change the site when required (e.g. if the site is red, hard, swollen, bleeding, leaking or painful).
- Turn the device off and remove the battery before cleaning.
- Store the device in a clean, dry area at room temperature.
(Queensland Health 2020a, 2021; BSPCC 2020)
Medicines
The four main medicines used to manage end-of-life symptoms are:
- Analgesics
- Sedatives
- Antiemetics
- Anticholinergics.
(palliAGED 2021)
Always ensure medicines are compatible before using them concurrently, both at the time of prescription and before administration (Queensland Health 2021).
Refer to the prescribing healthcare professional and Safer Care Victoria’s Syringe Driver Compatibility Guidance Document for detailed advice on medicine compatibility.
Complications
There are a variety of complications that may occur when using a syringe driver:
| Skin site complications |
|
| Medicine complications |
|
| Device complications |
|
| Other complications |
|
(Queensland Health 2021)
For specific guidance on how to manage these complications, refer to the instruction manual of your device and your local policies and procedures.
The Patient and Family Experience

Perceptions of syringe drivers vary; while they can be a positive experience for some, others may associate the device with a poor prognosis or a ‘transition to dying’. Understandably, the commencement of subcutaneous infusion may therefore be quite distressing for the patient and their family (Queensland Health 2021).
The device itself may also interfere with daily activities such as dressing, showering and sleeping (Queensland Health 2020a).
Therefore, it’s important to consider how patients and their families are feeling, educate them and provide emotional support where necessary. This may help to improve the outcomes of the infusion and instil confidence in patients and their families (Queensland Health 2021).
Remember to explain the following:
- Exactly what the device does
- Its benefits and potential disadvantages
- Safety principles
- How to care for the device
- Practical tips for managing the device during everyday life
- What the syringe driver means for the patient in the future (e.g. prognosis)
- Advance care planning and advance care directives (if applicable).
(Queensland Health 2021; BPAC NZ 2012)
Addressing any worries or concerns the patient and/or their family have about the syringe driver is also important. If appropriate to do so, you might need to reassure them that using a syringe driver doesn’t necessarily mean that death is imminent and that it will not speed up the dying process (BPAC NZ 2012).
Test Your Knowledge
Question 1 of 3
Which one of the following insertion sites would be the preferred choice in most cases?
Topics
References
- Best Practice Advocacy Centre New Zealand 2012, ‘When and How to Use a Syringe Driver in Palliative Care’, Best Practice Journal, viewed 23 January 2024, https://bpac.org.nz/bpj/2012/november/syringedrivers.aspx
- Brisbane South Palliative Care Collaborative 2020, A Practical Handbook For Health Professionals: How to Safely Set Up, Commence and Provide Necessary Documentation for NIKI T34TM Syringe Pump (2nd and 3rd Editions) Infusions, BSPCC, viewed 23 January 2024, https://www.caresearch.com.au/portals/10/Documents/NIKI-pump-practical-handbook-WEB.pdf
- CareSearch 2021, Syringe Drivers, CareSearch, viewed 23 January 2024, https://www.caresearch.com.au/tabid/6307/Default.aspx
- North Metropolitan Health Service 2021, Niki t34 Syringe Pump: Continuous Subcutaneous Infusion Management, Western Australian Government, viewed 23 January 2024, https://www.kemh.health.wa.gov.au/~/media/HSPs/NMHS/Hospitals/WNHS/Documents/Clinical-guidelines/Obs-Gyn-Guidelines/Palliative-Niki-T34-Syringe-Pump.pdf?thn=0
- palliAGED 2021, Syringe Drivers, palliAGED, viewed 23 January 2024, https://www.palliaged.com.au/tabid/4326/Default.aspx
- Queensland Health 2021, Guidelines for Subcutaneous Infusion Device Management in Palliative Care and Other Settings, Queensland Government, viewed 25 January 2022, https://www.health.qld.gov.au/__data/assets/pdf_file/0029/155495/guidelines.pdf
- Queensland Health 2018, Management of Subcutaneous Infusions in Palliative Care: Introduction, Queensland Government, viewed 23 January 2024, https://www.health.qld.gov.au/cpcre/subcutaneous/intro
- Queensland Health 2020a, Management of Subcutaneous Infusions in Palliative Care: Section 1: The Patient and Family/Carer Experience, Queensland Government, viewed 23 January 2024, https://www.health.qld.gov.au/cpcre/subcutaneous/section1
- Queensland Health 2020b, Management of Subcutaneous Infusions in Palliative Care: Section 3: Selection and Preparation of the Site, Queensland Government, viewed 23 January 2024, https://www.health.qld.gov.au/cpcre/subcutaneous/section3
- South Eastern Sydney Local Health District 2022, Administration of Subcutaneous Medications in Palliative Care, New South Wales Government, viewed 23 January 2024, https://www.seslhd.health.nsw.gov.au/node/8952
 New
New 
