Introduction
In the ever-evolving healthcare landscape, navigating complex clinical challenges is an everyday reality. The recent medication transcription and dispensing error clinical alert from the Aged Care Quality and Safety Commission has triggered questions, concerns, and the immediate need for revaluation.
If you’re wondering, ‘Where do I start?’ amidst this news, you're not alone. Events like this can put the already-challenged aged care sector into a state of uncertainty. Constrained by time and resources, the path to enable change and minimise any similar errors can appear daunting. But it is crucial to view these moments as catalysts — triggers for learning, change, and improvement.
Today’s Ausmed Guide aims to alleviate the mounting burden by offering ways to respond to this alert, from conducting a learning needs assessment to rethinking your educational approach. With this guide you can implement necessary changes that not only prevent medication transcribing and dispensing errors from happening at your facility, but also contributes to an overall improvement in resident care.
Step 1: Begin your learning needs assessment
It is natural to first turn towards education, asking questions such as: Are the staff adequately trained? Is more training needed?
Starting with a learning needs assessment is often the best way to approach this. This involves:
Understanding the root cause of errors: What factors led to this medication error?
Finding the gaps in current conditions. What safeguards are currently missing that could’ve prevented this?
Pinpointing the changes needed: What changes to learning can we implement to stop this from happening in future?
Using these systematic questions allows you to uncover not only the causes of errors, but also the gaps in learning and the changes required. It is also essential to acknowledge the broader context of the facility, encompassing all stakeholders, operational systems, and educational needs to prevent future incidents.
Step 2: Engage with people
Engaging with people can be the most valuable source of information. In an ideal world, discussions with stakeholders such as nursing staff, residents and their families would be a cornerstone in responding to any critical event. their experiences and their insights can provide critical context you won't find in any manual or guide. But aged care facilities are high-pressure environments with time at a premium. The challenge lies in finding key moments and snippets of time to gather your essential insights.
Staff
Find moments for a quick check-in at the start of a shift, or an impromptu chat as you help a carer make a bed. These moments can uncover uncertainties, hesitation, or even recurring issues with processes or systems.
For example, as you co-sign on a medication run, ask your nurse about their thoughts on the medication management system. This could reveal a recurring issue with system, such as a confusing interface, leading to delays or errors in updating medication records.
Emphasising psychological safety during these short interactions is key, to ensure staff feel at ease voicing their concerns. This can be achieved by framing questions in a way that emphasises learning, not blaming, such as 'What can we do better?' or 'How can we support you more effectively?'. This is the type of environment that encourages continuous improvement, growth and a culture of safety.
Quality
Your needs assessment can also provide an opportunity to identify gaps between the quality and education team. Although each department contributes to the overall quality of care, sometimes siloing does occur, especially in a busy aged care facility.
However, in light of events such as this medication transcribing and dispensing error, it is always important to ask the question: are education and quality working in harmony?
This question could expose gaps in communication or alignment. In your next cross-department meeting, you could add an agenda item to address the latest clinical alerts. This cross-department collaboration can improve system robustness and education requirements in parallel.
Step 3: Present your findings to improve systems
While it may be beyond the immediate responsibility of an L&D manager to directly modify systems or processes, understanding their impact is key to developing effective training and education for your staff.
As part of your learning needs analysis, it is important to engage with system owners to assist you in carrying out a thorough analysis of existing data and systems. Work with them to analyse past incident reports, complaint logs, and audit findings, which can help you identify systemic issues that inform training and education.
For example, if your facility is transitioning from tangible to digital medication management systems, it is important to work with system owners to identify the challenges staff are facing. Their challenges are not simply about learning a new tool or system; it’s a fundamental shift in care delivery.
Although new technology streamlines processes and improves accuracy, they can also create stress and uncertainty. Recognising this, it is important to work with system owners to create an environment where learning can take place at an organic pace, rather than add additional stress. Rushing or forcing the transition can lead to errors and frustration, especially when staff are under existing pressure.
Step 4: Revitalise your training plan
After understanding the challenges existing system and staff face regarding medication management, and going wide and engaging other stakeholders to assist in further querying system and processes, the heart of your response as an expert in learning and development lies a critical responsibility: reshaping your facility’s educational approach to bridge gaps and foster competency.
Aligning your approach to models like Miller's Pyramid can provide valuable guidance, particularly for an in-flux process such as medication management.
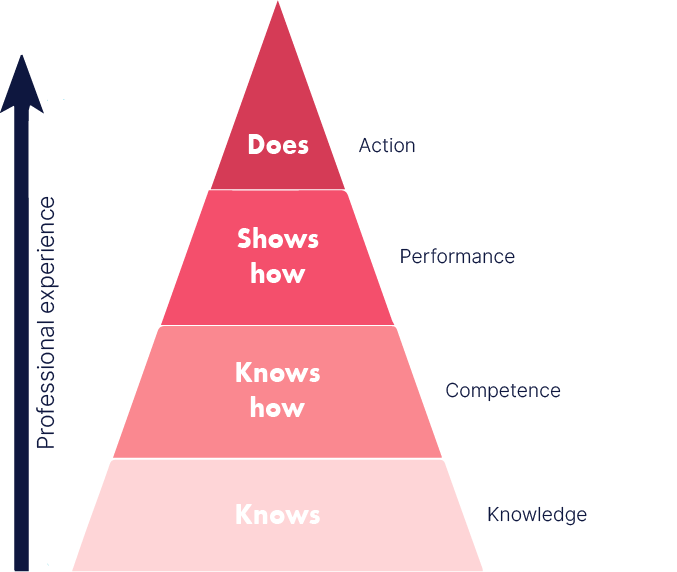
Built on the four stages of knowledge, competence, performance, and action, Miller’s Pyramid illuminates some of the challenges particular to medication management. It pushes us beyond the question, ‘Do our staff know this?' but instead to the more vital inquiries of ‘Can they apply what they know?’ and 'Are they given the opportunity to do so?’ With the transition to electronic medication management systems the need for knowledge is evident, but equally important, if not more important, is providing the opportunity for staff to apply, practise, and become comfortable with these new tools.
It's here that a robust training plan plays a pivotal role. Identifying areas that would benefit from additional training can guide your approach to education. From retraining staff on the electronic systems to revising medication protocols, your actions can strengthen the practical application of knowledge, promoting not just understanding but competency.
Conclusion
In our quest for quality and safety in aged care, responding to challenges like the recent medication transcription error alert necessitates a comprehensive strategy. By implementing a learning needs assessment, engaging stakeholders, reviewing systems, and revitalising educational strategies, we can foster an environment conducive to improvement and error prevention.
The Ausmed LMS survey tool can assist you in identifying the learning required for your staff. You can build out a set of questions that allows you to engage and query staff on their confidence around medication management. Select “Needs Assessment” and ask your staff questions such as:
On a scale of 1-10, how confident are you in using the current medication management system?
On a scale of 1-10, how comfortable are you with the transition from paper-based to electronic medication management systems?
Is there anything about the new electronic system that you find confusing or unintuitive?
Do you feel you have enough time during your shift to adequately manage medications?
What additional training, if any, do you believe would help you better manage medication?
Furthermore, our extensive content library will serve as a resource to complement your findings, providing learning modules specifically designed around error prevention and efficient medication management. These include:
At Ausmed, we support you in this journey. We want to empower you to have a comprehensive and responsive educational strategy that meets the needs of your staff and the complex challenges they face. Reach out to your Ausmed customer support specialist.



