I present in shades of pigment - from black, to skin-toned. My size ranges from millimetres to centimetres. Flat and masquerading as a freckle, or raised and mole-like, I may be completely symptomless. I am melanoma.
While melanoma is a serious and potentially life-threatening type of skin cancer, it can be effectively treated if addressed quickly enough (MIA 2023a).
For this reason, being able to detect and treat melanoma early is crucial - especially in Australia and New Zealand, where melanoma rates are the highest in the world (Cancer Council Victoria 2021).
Melanomas have several features distinguishing them from other skin cancers. Awareness of these differences can assist with timely referral and treatment, thereby reducing morbidity associated with aggressive tumours and enhancing overall patient outcomes. All healthcare professionals should be able to identify lesions and refer appropriately.
What is Melanoma?
Melanoma is the third most common type of cancer in Australia (excluding non-melanoma skin cancers e.g. basal cell carcinoma (BCC) and cutaneous squamous cell carcinoma (cSCC)) (Cancer Council Australia 2022).
Due to its ability to grow and spread quickly - with the potential to become life-threatening in as little as six weeks - it is considered the most serious type of skin cancer (SunSmart 2014).
If untreated, melanoma can spread rapidly to other areas of the body, including the lungs, brain, liver or bones through the lymphatic system or bloodstream (MIA 2023a).
How Does Melanoma Develop?
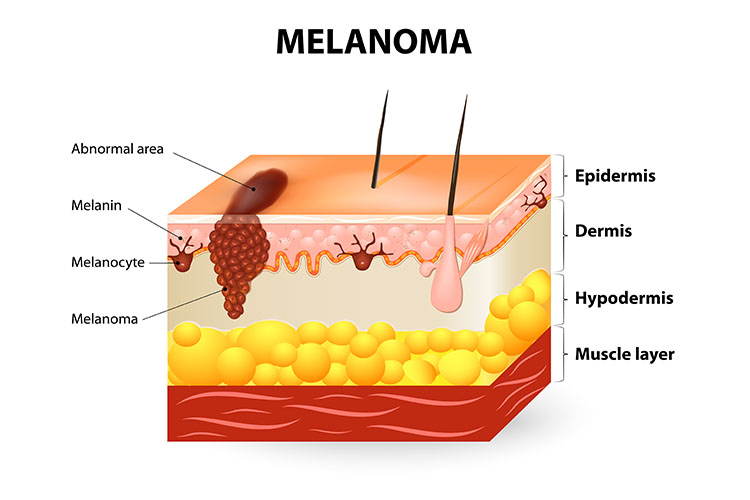
Melanoma is triggered by DNA mutation (caused by UV radiation, usually from the sun) to the melanocyte cells, which sit in the basal cell layer of the epidermis (Skin Cancer Foundation 2022; Cancer Council Victoria 2021).
Melanocytes help to protect the skin by producing melanin (pigment) upon exposure to UV radiation. In some cases, melanocytes cluster together during this process and form nevi (moles). DNA damage from burning or tanning can cause the melanocytes to mutate and grow in an uncontrolled way (MIA 2023a; Skin Cancer Foundation 2022).
It’s possible for a previously benign mole to develop into a melanoma, but about a third of melanomas occur in this way. It’s more common for melanomas to appear as completely new lesions (MIA 2023a).
Melanomas usually develop in areas that are frequently exposed to UV radiation, such as the face, back, arms and legs, but they can appear anywhere on the body. This includes areas like the soles of the feet, the genitals, the nails and the inside of the mouth and eyes that receive very little UV exposure (Mayo Clinic 2023; MIA 2023a; Cancer Council Australia 2023).
Warning Signs for Melanoma
Melanomas can be a variety of sizes, shapes and colours. In most cases, they present as new and unusual-looking lesions. They may be several millimetres or centimetres in diameter, depending on how much they have grown. Common characteristics include an uneven or smudgy outline, blotchiness, and a flat or slightly raised surface. Existing moles that develop into melanomas will often change in colour, size or shape (SunSmart 2014; Seebacher 2022).
Possible colours include brown, black, blue, red and grey, or several of these colours within the one lesion. Some melanomas may be amelanotic, meaning they lack pigment (Seebacher 2022).
They may be itchy or tender, and some crust or bleed (Seebacher 2022).
Types of Melanoma
| Type | Prevalence | Location | Common physical characteristics | Growth and spread rate | Image |
|---|---|---|---|---|---|
| Superficial spreading melanoma |
|
|
|
Grows slowly, but can be dangerous if it progresses |  |
| Nodular melanoma |
|
Usually found on the head and neck | Raised, round nodule on the surface of the skin | Fast-growing and aggressive |  'Photography of nodular melanoma' by DermNetNZ is licensed under CC BY 4.0 |
| Lentigo maligna melanoma |
|
Usually appears on the face, ears, head or neck |
|
Grows slowly and close to the surface of the skin |  'Lentigo maligna melanoma on the left cheek' by Omar Bari & Philip R. Cohen is licensed under CC BY 3.0 |
| Acral lentiginous melanoma |
|
Usually appears in ‘hidden’ areas including under the nails, on the soles of feet and on the palms of hands |
|
Grows slowly before becoming invasive |  'Photography of a large acral lentiginous melanoma' by Xavier-Júnior; José & Munhoz; Tania & Souza; Vinicius & Campos; Eloísa & Stolf; Hamilton & Marques; Mariângela is licensed under CC BY 4.0 |
| Desmoplastic melanoma |
|
Usually appears on the head or neck |
|
Grows and changes over time |
(Cancer Council Victoria 2021; Skin Cancer Foundation 2022; Oakley 2017)
Prevalence of Melanoma
Annually, melanoma is estimated to affect 16,800 Australians and cause 1,300 deaths (MIA 2022a).
As a comparison, there are over one million treatments performed anually for non-melanoma skin cancers in Australia, and cSCC and BCC combined cause about 560 deaths annually (Cancer Council Australia 2019, 2022).
It is estimated that about 1 in 14 men and 1 in 21 women will develop melanoma before the age of 85. While the average age of diagnosis is in a person’s 60s, people of any age can develop melanoma, with those under 40 making up about 8% of cases (Cancer Council Australia 2022).
Risk Factors for Melanoma
- Older age
- Fair complexion (particularly if the individual has freckles, blonde or red hair or blue or green eyes)
- Lots of moles (more than 10 above the elbow on the arms and more than 50 on the body), especially if they are irregular or uneven
- History of skin cancer (melanoma or another type)
- Strong family history of melanoma
- Unprotected UV exposure (either from the sun or artificial sources)
- Short, intense periods of UV exposure
- History of sunburns or tanning
- Reduced immune function due to illness or immunosuppressive medications
- Parkinson’s disease.
(Cancer Council Victoria 2021; Seebacher 2022)
Diagnosis and Treatment of Melanoma

Appromxiately 90% of melanomas can treated with surgery if caught early. Therefore, early recognition is crucial (MIA 2022b).
ABCDE Guidelines
The ABCDE guidelines can be used to assess a lesion for possible melanoma.
| A: Asymmetry | One half of the lesion is different from the other in shape, structure or colour. |
| B: Border irregularity | The edges of the lesion are irregular, ragged, notched or blurred. |
| C: Colour variation | There are several different colours within the lesion that may be unevenly or irregularly distributed. |
| D: Diameter | The lesion is larger than 6 mm in diameter or is noticeably growing. |
| E: Evolving | The lesion is changing in size, shape, colour or elevation, or is itching, bleeding or crusting. |
(MIA 2022b; Jin 2021)
If melanoma is suspected, the patient will generally undergo a biopsy (either partial or excisional) and the skin sample will be sent for a pathological assessment (MPA 2022a).
Melanoma Staging and Treatment
| Stage | Thickness | Spread | Main treatment options | |
|---|---|---|---|---|
| Stage 0 (in situ) |
|
|
|
|
| Stage I | IA |
|
|
|
| IB |
|
|||
| Stage II | IIA |
|
|
|
| IIB |
|
|||
| IIC |
|
|||
| Stage III | IIIA |
|
|
|
| IIIB | ||||
| IIIC | ||||
| IIID | ||||
| Stage IV |
|
|
|
|
(MPA 2022b; Cancer Council NSW 2023; MIA 2023b)
Conclusion
While melanomas can usually be resolved through excision if caught early enough, untreated melanomas can quickly become complicated and life-threatening.
Therefore, being able to identify and respond to suspect lesions as soon as possible is crucial.
Test Your Knowledge
Question 1 of 3
What does the term ‘amelanotic’ refer to?
Topics
References
- Cancer Council Australia 2023, Melanoma, Cancer Council Australia, viewed 16 August 2023, https://www.cancer.org.au/cancer-information/types-of-cancer/melanoma
- Cancer Council Australia 2019, Clinical Practice Guidelines for Keratinocyte Cancer > 6. Prognosis, Cancer Council Australia, viewed 16 August 2023, https://wiki.cancer.org.au/australia/Guidelines:Keratinocyte_carcinoma/Prognosis
- Cancer Council Australia 2022, Skin Cancer Incidence and Mortality, Cancer Council Australia, viewed 16 August 2023, https://wiki.cancer.org.au/skincancerstats/Skin_cancer_incidence_and_mortality
- Cancer Council Victoria 2021, Melanoma, Cancer Council Victoria, viewed 16 August 2023, https://www.cancervic.org.au/cancer-information/types-of-cancer/melanoma/melanoma-overview.html
- Jin, Q 2021, ABCDEs of Melanoma, DermNet, viewed 16 August 2023, https://dermnetnz.org/topics/abcdes-of-melanoma/
- Mayo Clinic 2023, Melanoma, Mayo Clinic, viewed 16 August 2023, https://www.mayoclinic.org/diseases-conditions/melanoma/symptoms-causes/syc-20374884
- Melanoma Institute Australia 2022b, Checking Your Skin, MIA, viewed 16 August 2023, https://melanoma.org.au/about-melanoma/checking-your-skin/
- Melanoma Institute Australia 2023b, Melanoma Diagnosis, MIA, viewed 16 August 2023, https://melanoma.org.au/for-patients/melanoma-diagnosis/
- Melanoma Institute Australia 2022a, Melanoma Facts, MIA, viewed 16 August 2023, https://melanoma.org.au/about-melanoma/melanoma-facts/
- Melanoma Institute Australia 2023a, What is Melanoma?, MIA, viewed 15 August 2023, https://www.melanoma.org.au/understanding-melanoma/what-is-melanoma/
- Melanoma Patients Australia 2022a, How is Melanoma Diagnosed?, MPA, viewed 16 August 2023, https://melanomapatients.org.au/diagnosis/how-is-melanoma-diagnosed/
- Melanoma Patients Australia 2022b, Staging Of Melanoma, MPA, viewed 16 August 2023, https://melanomapatients.org.au/staging-of-melanoma/
- Seebacher, NA 2022, Melanoma, DermNet, viewed 16 August 2023, https://dermnetnz.org/topics/melanoma
- Skin Cancer Foundation 2022, Melanoma Overview, Skin Cancer Foundation, viewed 16 August 2023, https://www.skincancer.org/skin-cancer-information/melanoma/
- SunSmart 2014, About Skin Cancer, SunSmart, viewed 16 August 2023, https://www.sunsmart.com.au/skin-cancer/about-skin-cancer
 New
New 
