One in 2,500 people (i.e. one birth every four days) is born with cystic fibrosis, making it the most common incurable, life-limiting disorder in Australia (Healthdirect 2023; Better Health Channel 2024).
What is Cystic Fibrosis?
Cystic fibrosis (CF) is a life-limiting genetic condition in which abnormally thick and sticky mucus is produced, causing complications that predominantly affect the respiratory, digestive and reproductive systems (Better Health Channel 2024).
CF is incurable and shortens life expectancy; however, this has rapidly improved in recent years due to improvements in care. Now, the average life expectancy is 49 years for people born between 2005 and 2009 and 56 years for people born between 2016 and 2020 (Monash University 2023).
How Does Cystic Fibrosis Affect the Body?
CF occurs due to a mutation in the cystic fibrosis transmembrane conductance regulator (CFTR) gene, which is responsible for coding the CFTR protein (CFF 2021a).
This mutation causes the CFTR protein - which is responsible for regulating the balance of salt and water on certain body surfaces (such as the lungs) - to behave abnormally. In some cases, the CFTR protein is not produced at all (CFF 2021a).
A normal CFTR protein allows chloride (a salt component) to move from the inside of a cell to the outside, where it attracts water to the cellular surface. This water allows tiny hairs on the cellular surface (known as cilia) to sweep mucus away (CFF 2021a).
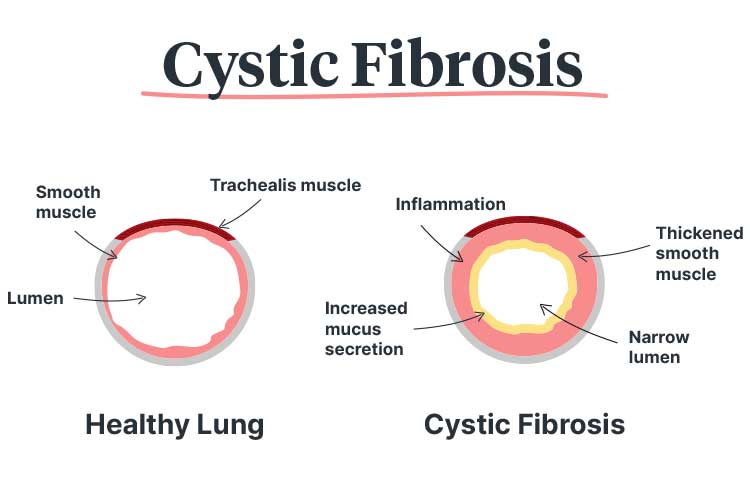
However, a defective or absent CFTR protein causes the chloride to become trapped inside the cells, preventing water from hydrating the cellular surfaces. As a result, the mucus dehydrates and becomes thicker. Furthermore, the cilia are weighed down by this thick mucus and are unable to sweep it away, causing it to accumulate (CFF 2021a).
This build-up of mucus is particularly dangerous in the lungs, as it clogs air passages and traps bacteria, leading to frequent blockages and infections. Over time, this may cause permanent lung damage (Better Health Channel 2024).
Accumulated mucus in the digestive system prevents digestive enzymes from being transferred between the pancreas and small intestine, causing issues with digesting fats and absorbing nutrients (Better Health Channel 2024).
How is Cystic Fibrosis Inherited?
CF is an autosomal recessive disease, meaning that it is not possible to inherit CF unless both parents have the defective gene (MedlinePlus 2021; Mayo Clinic 2024a).
A person who inherits only one defective gene (i.e. from only one parent) is a carrier but will not show symptoms, as the normal (unaffected gene) is dominant and will be able to compensate for the defect (Mayo Clinic 2024a).
Therefore, if both parents are carriers:
- There is a 25% chance that the child will be unaffected
- There is a 50% chance that the child will be a carrier
- There is a 25% chance that the child will have CF.
(Mayo Clinic 2024a)
If one parent has CF and the other is a carrier:
- There is a 50% chance that the child will be a carrier
- There is a 50% chance that the child will have CF.
(CFF 2021c)
It is estimated that 1 in 25 Australians are carriers. While most carriers are unaware that they have the defective gene, screening services are available (Cystic Fibrosis Australia 2023).
Autosomal recessive conditions like CF can skip generations (Cystic Fibrosis Australia 2023).
Symptoms of Cystic Fibrosis
CF affects the body in a variety of ways and may cause:
- A persistent cough that may produce mucus
- Breathing issues
- Wheezing
- Frequent lung infections and sinusitis
- Salty sweat
- Muscle cramps or weakness in hot weather due to salt loss in sweat
- Fatigue
- Difficulty gaining weight
- Frequent toilet visits
- Bulky, greasy stools
- Diarrhoea or constipation
- Decreased appetite.
(Better Health Channel 2024)
Patients with CF often experience acute worsening of respiratory symptoms (known as pulmonary exacerbations (PEx)). PEx episodes often involve symptoms such as increased mucus production, increased coughing and shortness of breath along with a decrease in lung function (CFF 2021d).
Complications of Cystic Fibrosis
People with CF may experience a variety of complications, including:
- Recurring lung infections
- Pulmonary exacerbations (acute worsening of respiratory symptoms)
- Bronchiectasis
- Haemoptysis (coughing up blood due to airway damage)
- Pneumothorax
- Respiratory failure
- Allergic bronchopulmonary aspergillosis (ABPA) (allergic reaction to fungus in the lungs)
- Cardiac failure from lung damage
- Cancer of the digestive tract
- Malnutrition
- Diabetes (affecting about 20% of teenagers with CF and up to 50% of adults with CF)
- Liver disease
- Kidney issues
- Pancreatitis
- Intestinal obstruction
- Distal intestinal obstruction syndrome (DIOS)
- Infertility (particularly in males)
- Osteoporosis
- Arthritis
- Electrolyte imbalances or dehydration
- Mental illness.
(Mayo Clinic 2024b; NHLBI 2024)
CF gradually damages lung tissue, decreasing lung function. In most cases, death is caused by eventual respiratory failure (NHLBI 2024; Yu et al. 2024).
Diagnosis of Cystic Fibrosis

Between 48 and 72 hours after birth, neonates can undergo a heel prick test to detect CF and other medical conditions. A suspected CF diagnosis can then be confirmed by measuring the infant’s sweat for a high concentration of sodium chloride at about six weeks of age (CF Together 2024; Healthdirect 2023).
Management of Cystic Fibrosis
CF is incurable and requires intensive management to slow its progression (Better Health Channel 2024).
This may include:
- Daily chest physiotherapy
- A variety of medicines, which may include CFTR modulators, antibiotics and pancreatic enzyme supplements
- Inhalation using a compressed air pump and nebuliser
- A balanced diet that contains high amounts of protein, fat and kilojoules
- Percutaneous endoscopic gastrostomy (PEG) (the insertion of a flexible feeding tube)
- Lung, liver or pancreas transplant
- Vitamins
- Salt supplements
- Frequent exercise
- Regular visits to a CF specialty clinic.
(Better Health Channel 2024; Healthdirect 2023; CFF 2021a)
Infection Prevention
The thick mucus caused by CF traps pathogens in the airway, causing frequent infections (Cleveland Clinic 2024).
For this reason, those with CF need to take measures to reduce the risk of infection such as:
- Practising effective hand hygiene
- Receiving all recommended vaccines, including yearly influenza shots (those who live with the patient should also receive these vaccinations)
- Avoiding close contact with other people who have CF.
(NHLBI 2024)
Caring for Patients With Cystic Fibrosis
People with CF have different care needs depending on their stage of life:
| Life stage | Care needs |
|---|---|
| Newly diagnosed |
|
| Children |
|
| Adolescents |
|
| Young adults |
|
| Adults |
|
| Those with severe disease |
|
(Adapted from ACI 2016)
Annual Comprehensive Review
All patients with CF require an annual health review at a CFSS facility. This should include the following assessments:
- Respiratory status
- Biochemistry
- Nutrition
- Psychosocial health
- Fertility and contraception (if applicable)
- Any procedures that have been performed
- Preventive health.
(ACI 2016)
Test Your Knowledge
Question 1 of 3
A woman who has CF is pregnant. Her partner is not a carrier. What is the likelihood that their child will inherit CF?
Topics
References
- Agency for Clinical Innovation 2016, Cystic Fibrosis, New South Wales Government, viewed 14 April 2025, https://aci.health.nsw.gov.au/__data/assets/pdf_file/0003/338124/ACI16125_Cystic_Fibrosis_MoC_F_web.pdf
- Better Health Channel 2024, Cystic Fibrosis (CF), Victoria State Government, viewed 14 April 2025, https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/cystic-fibrosis-cf
- Cystic Fibrosis Australia 2023, Causes of CF, Cystic Fibrosis Australia, viewed 14 April 2025, https://www.cysticfibrosis.org.au/causes/
- CF Together 2024, How Cystic Fibrosis Diagnosed?, CF Together, viewed 14 April 2025, https://www.cftogether.org.au/understanding-cf/diagnosis
- Cleveland Clinic 2024, Cystic Fibrosis, Cleveland Clinic, viewed 14 April 2025, https://my.clevelandclinic.org/health/diseases/9358-cystic-fibrosis
- Cystic Fibrosis Foundation 2021a, About Cystic Fibrosis, Cystic Fibrosis Foundation, viewed 14 April 2025, https://www.cff.org/What-is-CF/About-Cystic-Fibrosis/
- Cystic Fibrosis Foundation 2021b, Basics of the CFTR Protein, Cystic Fibrosis Foundation, viewed 14 April 2025, https://www.cff.org/research-clinical-trials/basics-cftr-protein
- Cystic Fibrosis Foundation 2021c, CF Genetics: The Basics, Cystic Fibrosis Foundation, viewed 14 April 2025, https://www.cff.org/What-is-CF/Genetics/CF-Genetics-The-Basics/
- Cystic Fibrosis Foundation 2021d, Pulmonary Exacerbations Clinical Care Guidelines, Cystic Fibrosis Foundation, viewed 14 April 2025, https://www.cff.org/Care/Clinical-Care-Guidelines/Respiratory-Clinical-Care-Guidelines/Pulmonary-Exacerbations-Clinical-Care-Guidelines/
- Healthdirect 2023, Cystic Fibrosis (CF), Australian Government, viewed 14 April 2025, https://www.healthdirect.gov.au/cystic-fibrosis-cf
- Mayo Clinic 2024a, Autosomal Recessive Inheritance Pattern, Mayo Clinic, viewed 14 April 2025, https://www.mayoclinic.org/autosomal-recessive-inheritance-pattern/img-20007457
- Mayo Clinic 2024b, Cystic Fibrosis, Mayo Clinic, viewed 14 April 2025, https://www.mayoclinic.org/diseases-conditions/cystic-fibrosis/symptoms-causes/syc-20353700
- MedlinePlus 2021, What Are the Different Ways in Which a Genetic Condition Can Be Inherited?, U.S. Department of Health and Human Services, viewed 14 April 2025, https://medlineplus.gov/genetics/understanding/inheritance/inheritancepatterns/
- Monash University 2023, ‘Huge Gains Seen in Life Expectancy for Australians with Cystic Fibrosis’, Medicine, Nursing and Health Sciences News, 17 January, viewed 14 April 2025, https://www.monash.edu/medicine/news/latest/2023-articles/huge-gains-seen-in-life-expectancy-for-australians-with-cystic-fibrosis
- National Heart, Lung, and Blood Institute 2024, Cystic Fibrosis, National Institutes of Health, viewed 14 April 2025, https://www.nhlbi.nih.gov/health-topics/cystic-fibrosis
- Yu, E, Sankari, A & Sharma, S 2024, ‘Cystic Fibrosis’, StatPearls, viewed 14 April 2025, http://ncbi.nlm.nih.gov/books/NBK493206/
 New
New