Early detection of neurological deterioration in patients means interventions are more likely to be successful (Shahrokhi & Asuncion 2023).
Therefore, you must be informed about the possible causes of neurological deterioration, know how to correctly assess the patient and intervene appropriately.
A decrease of more than 2 points on the Glasgow Coma Scale (GCS), which measures a patient's level of consciousness on a scale of 3 to 15, is a warning sign of neurological deterioration (Shkirkova et al. 2018; Trauma Victoria 2024).
Patients may present with varying levels of consciousness, ranging from full alertness and awareness to some level of impairment to complete unawareness and unresponsiveness (Cooksley et al. 2018).
A patient with a GCS score of less than 8 is considered to be neurologically compromised, which is a medical emergency relying on prompt diagnosis and medical management for a favourable patient outcome (Cooksley et al. 2018).
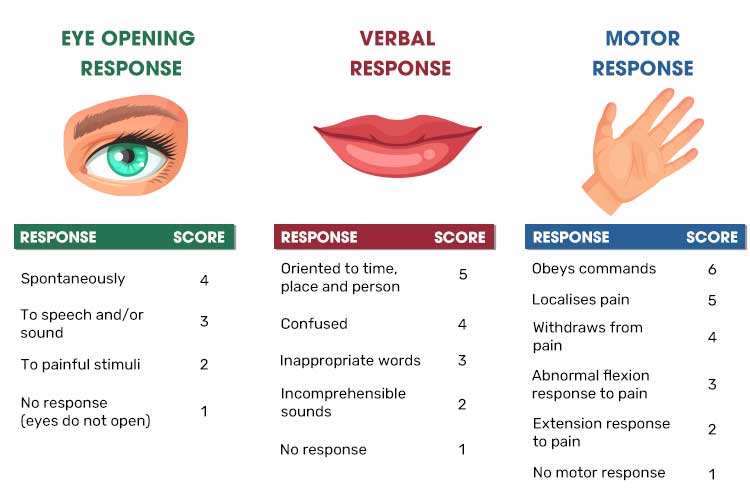
Read: Neurological Assessment and GCS
Common Causes of Neurological Deterioration
While a neurological assessment is useful for recognising deterioration, the cause will need to be identified so that the patient can be appropriately treated. The following are some common causes of neurological deterioration:
Sedation
Sedation-related neurological deterioration may be caused by opiate overdose or anaesthetic that has not been reversed effectively, causing the patient to remain heavily sedated.
The patient may present with:
- Pinpoint pupils
- Respiratory decline or a decrease in respiratory rate - this may cause apnoea, which is a medical emergency
- Drowsiness or unresponsiveness (in the case of opiate overdose)
- Airway obstruction or hypoxia (may occur if an anaesthetic has not been reversed appropriately), hindering the ability of a person to breathe on their own.
(Vincent et al. 2018; Regina et al. 2025)
Stroke
Neurological deterioration may be caused by:
- Ischaemic stroke
- Haemorrhagic stroke
- A space-occupying lesion.
The patient’s pupils may appear unequal. A stroke is a medical emergency and requires early recognition, treatment and intervention.
(Jeffery et al. 2019; Stroke Foundation 2025)
Seizure
A patient experiencing a seizure may present with mydriasis (dilated pupils) (Epilepsy Action Australia 2024).
In the case of a seizure, protect the patient and call for assistance.
Hypoglycaemia
Hypoglycaemia (abnormally low glucose levels) can cause neurological deterioration, as the brain relies on blood glucose for energy (Harvard Health Publishing 2022). It may be caused by:
- Fasting
- Poor nutrition
- Administration of insulin
- Medications
- Excessive alcohol consumption
- Endocrine disorders.
(Brutsaert 2024)
Other Causes
Other causes of neurological deterioration include:
- Traumatic brain injury
- Tumour
- Lack of oxygen (e.g. from drowning or a heart attack)
- Infection
- Toxins (e.g. carbon monoxide)
- Drugs and alcohol.
(Mayo Clinic 2024)
Managing Neurological Deterioration
- Assess the patient using the GCS in conjunction with a head-to-toe assessment.
- Assess the patient’s level of consciousness.
- Ensure the patient is free from any environmental danger. If the patient is on the floor, call for assistance and only move them to the bed if they are haemodynamically stable and all manual handling equipment is available.
- Support the patient’s respiratory demands.
- Increase the frequency of observations.
- Coordinate relevant scans and tests.
- Implement 3 or 5-lead cardiac monitoring if appropriate.
- Optimise oxygenation and perfusion status.
- Perform basic life support if required.
- Care may need to be escalated to critical care services.
(NSW Health 2025; Park & Kellerman 2022; ACSQHC 2021)
Complications
- The patient may be unable to protect their own airway - this is an emergency situation.
- If the patient is unresponsive, commence basic life support.
- If a post-collapse injury occurs, escalate care as required.
- Consider critical care admission if required.
(NSW Health 2025; Park & Kellerman 2022; ACSQHC 2021)
Conclusion
Early detection of neurological deterioration contributes to successful intervention and favourable patient outcomes. Ensure you:
- Treat the patient’s signs and symptoms promptly
- Increase the frequency of observation
- Identify the cause of the deterioration
- Correct any metabolic and electrolyte imbalances
- Support the patient’s haemodynamic status.
(NSW Health 2025; Park & Kellerman 2022; ACSQHC 2021)
Note: This article is intended as a refresher and should not replace best-practice care. Always refer to your facility's policy on recognising and responding to acute neurological deterioration.
Test Your Knowledge
Question 1 of 3
What change to a patient’s GCS score might indicate neurological deterioration?
Topics
Further your knowledge
References
- Australian Commission on Safety and Quality in Health Care 2021, National Consensus Statement: Essential Elements for Recognising and Responding to Acute Physiological Deterioration, 3rd edn, Australian Government, viewed 26 May 2025, https://www.safetyandquality.gov.au/publications-and-resources/resource-library/national-consensus-statement-essential-elements-recognising-and-responding-acute-physiological-deterioration-third-edition
- Brutsaert, EF 2024, Hypoglycemia, MSD Manual, viewed 21 May 2025, https://www.msdmanuals.com/home/hormonal-and-metabolic-disorders/diabetes-mellitus-dm-and-disorders-of-blood-sugar-metabolism/hypoglycemia?query=Hypoglycemia#v773444
- Cooksley, T, Rose, S & Holland, M 2018, ‘A Systematic Approach to the Unconscious Patient’, Clin Med (Lond)., vol. 18 no. 1, viewed 21 May 2025, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6330912/
- Epilepsy Action Australia 2024, Recognising Seizure Stages, Epilepsy Action Australia, viewed 21 May 2025, https://www.epilepsy.org.au/about-epilepsy/understanding-epilepsy/seizure-stages/
- Harvard Health Publishing 2022, Hypoglycemia, Harvard Medical School, viewed 21 May 2025, https://www.health.harvard.edu/a_to_z/hypoglycemia-a-to-z
- Jeffery, RCH, Young, B, Swann, PG & Lueck, CJ 2019, ‘Unequal Pupils’, Australian Journal of General Practice, vol. 48, no. 1-2, viewed 21 May 2025, https://www1.racgp.org.au/getattachment/26f85d1e-c084-4ae7-ac27-58839cd3d0b1/Unequal-pupils.aspx
- Mayo Clinic 2024, Coma, Mayo Clinic, viewed 21 May 2025, https://www.mayoclinic.org/diseases-conditions/coma/symptoms-causes/syc-20371099
- NSW Health 2025, Recognition and Management of Patients Who Are Deteriorating, New South Wales Government, viewed 26 May 2025, https://www1.health.nsw.gov.au/pds/ActivePDSDocuments/PD2025_014.pdf
- Park, SA & Kellerman, T 2022, ‘Acute Nursing Care: Recognition and Response to Deteriorating Patients’, ANMJ, 8 July, viewed 26 May 2025, https://anmj.org.au/acute-nursing-care-recognition-and-response-to-deteriorating-patients-2/
- Regina, AC, Goyal, A & Mechanic, OJ 2025, ‘Opioid Overdose’, StatPearls, viewed 21 May 2025, https://www.ncbi.nlm.nih.gov/books/NBK470415/
- Shahrokhi, M & Asuncion, RMD 2023, ‘Neurologic Exam’, StatPearls, viewed 21 May 2025, https://www.ncbi.nlm.nih.gov/books/NBK557589/
- Shkirkova, K, Saver, JL, Starkman, S et al. 2018, ‘Frequency, Predictors, and Outcomes of Prehospital and Early Postarrival Neurological Deterioration in Acute Stroke’, JAMA Neurology, viewed 21 May 2025, https://jamanetwork.com/journals/jamaneurology/fullarticle/2688300
- Stroke Foundation 2025, Living Clinical Guidelines for Stroke Management, Stroke Foundation, viewed 21 May 2025, https://informme.org.au/guidelines/living-clinical-guidelines-for-stroke-management
- Trauma Victoria 2024, The Deteriorating Trauma Patient: Clinical Observation of Major Trauma Patient, Victoria State Government, viewed 21 May 2025, https://trauma.reach.vic.gov.au/guidelines/the-deteriorating-trauma-patient/clinical-observation-of-major-trauma-patient
- Vincent, J, Einav, S, Pearse, R et al. 2018, ‘Improving Detection of Patient Deterioration in the General Hospital Ward Environment’, Eur J Anaesthesiol., vol. 35 no. 5, viewed 21 May 2025, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5902137/
 New
New