Focus on Skin Cancer: An Overview
Published: 21 November 2023

Published: 21 November 2023

The start of summer in Australia is an important time for nurses to turn their focus to the skin.
Australia has one of the highest skin cancer rates worldwide, with the Cancer Council Australia (2022) forecasting that at least two out of three Australians will be diagnosed with skin cancer in their lifetime. Luckily, skin cancer is visible, mostly preventable and curable when detected and treated early.
Though the rates of skin cancer diagnoses are forecast to increase, the stable figures for individuals under the age of 45 currently reflect Australia’s long-standing public education on UV (ultraviolet) avoidance and protection (Cancer Council Australia 2022).
Nurses should expect to care for individuals with sun-damaged skin who have an increased risk of developing skin cancer, possibly incidental to their primary reason for care. In addition to the physical concerns, the psychosocial ramifications of skin cancer following diagnosis are well documented. Anxiety and depression may stem from the fear of actual or anticipated disfigurement, multiple surgeries and treatments. Financial costs, disrupted social relationships and impaired lifestyle add to the burden.
Effective nurse participation in skin cancer recognition, prevention and management, as well as patient support and guidance along recognised referral pathways, requires a basic knowledge and understanding of melanoma and non-melanoma skin cancer.
The three main types of skin cancer originate from epidermal cell genetic mutation:
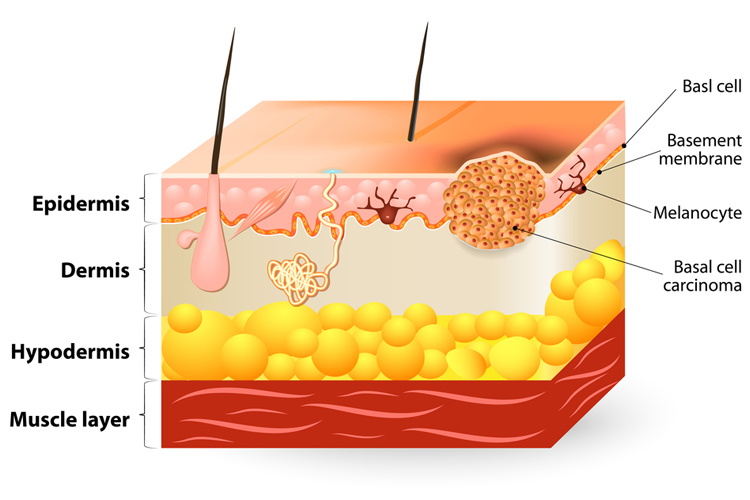
Basal Cell Carcinomas (BCC) derive from stem cells located in the epidermal basal layer or hair follicles.
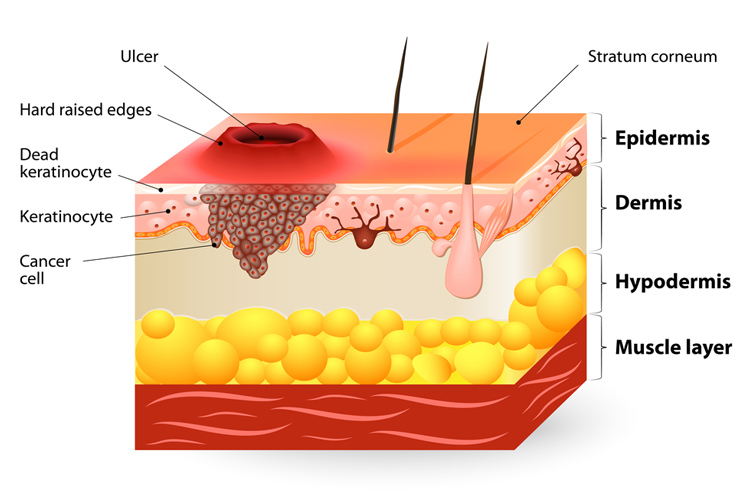
Squamous Cell Carcinomas (SCC) develop from keratinocytes.
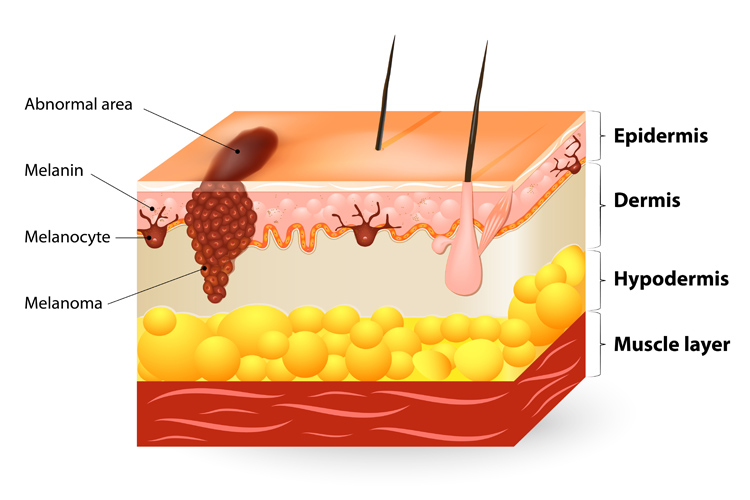
Melanomas advance from melanocytes, basal layer pigment-producing cells.
BCCs may display a classic rolled edge or central indentation; alternatively, there may be a pearly bump, red patch, pink growth or a pale, firm, scar-like lesion. SCCs, on the other hand, often appear as a scaly lump that ulcerates (Skin Cancer Foundation 2022). They may also present as a keratotic horn (Oakley 2015).
Melanoma may present as a new or changing lesion, usually pigmented, with colour variation. Its appearance may differ from other pigmented lesions on the person (Cancer Council Australia 2023). BCCs, SCCs and melanomas can present in sub-types. Though each skin cancer has classic characteristics, they may vary from the description usually attributed to them. Specific tumour behaviour, treatment choice and outcome potential also depend on the specific type.
Subtleties in appearance may impact the accuracy and timeliness of diagnosis, care flow, health resources and patient morbidity and mortality.
For instance, the ABCDE rule applies when identifying some suspicious pigmented lesions:
(Jin 2021)
However, you must be aware that in paediatrics, nodular or amelanotic melanoma, the individual might not present with conventional ABCDE criteria for diagnosing a suspicious lesion or melanoma.

There are a number of risk factors around skin cancer that should be taken into account:
(Mayo Clinic 2022)
Nurses are well-positioned to have a positive impact on community skin cancer awareness and to advise on sun protection and minimisation techniques. Wherever you work as a nurse, you have a role in the education, prevention and management of skin cancers.
Greater nurse knowledge and awareness increases vigilance, aids early identification and improves patient outcomes. Irrespective of care context, it is best to approach suspicious or new lesions and non-healing wounds with a level of wariness.