Diarrhoea is a common condition that generally doesn’t indicate a serious underlying issue. However, it can be an uncomfortable and unpleasant experience (NHS Inform 2023).
What is Diarrhoea?
Diarrhoea is defined as passing more than three loose, watery stools within one day (or more frequent passage than is typical for the individual) (Healthdirect 2024a).
Diarrhoea is when more than three loose, watery stools are passed within one day (Healthdirect 2019a).
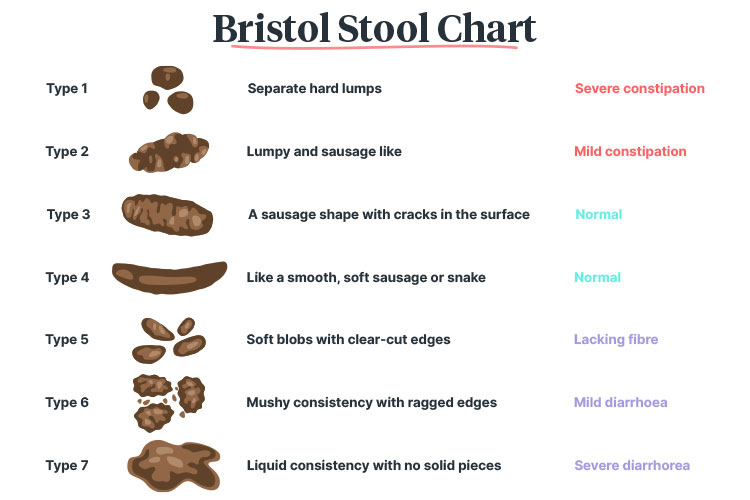
Generally, the stools passed by someone experiencing diarrhoea are between type 5 and type 7 on the Bristol Stool Chart (Continence Health Australia 2024).
Diarrhoea may be either:
- Acute, lasting for up to two weeks (but generally resolving on its own within 1 to 2 days), or
- Chronic, lasting for over four weeks.
(Better Health Channel 2023)
It is common for adults to experience one episode of acute diarrhoea every year (MedlinePlus 2025).
The Physiology of Diarrhoea
During the digestion process, the small and large intestines absorb nutrients and fluid from food that has been consumed (Bladder & Bowel Community 2024). The remaining substance then becomes waste (faeces) and is excreted. Generally, stools are between 60% and 90% water (Gotfried 2024).
Diarrhoea occurs when less fluid than usual is absorbed from the waste or when there is increased fluid secretion from the intestines (Gotfried 2024).
Causes of Diarrhoea
Acute Diarrhoea
Most cases of acute diarrhoea are caused by infections such as gastroenteritis (Nemeth & Pfleghaar 2022). Potential causative pathogens include:
- Viruses (e.g. norovirus, rotavirus)
- Bacteria (e.g. Campylobacter, Clostridium difficile (C. difficile), Escherichia coli (E. coli))
- Parasites (e.g. Giardia, cryptosporidium).
(Healthdirect 2024b; Nemeth & Pfleghaar 2022)
It is estimated that one-fifth of all infectious diarrhoea cases are caused by norovirus (Nemeth & Pfleghaar 2022).
Other causes of acute diarrhoea include:
- Contaminated food or water from overseas (known as ‘traveller’s diarrhoea’)
- Food poisoning
- Anxiety or distress
- Excess alcohol
- Appendicitis
- Certain medicines (e.g. antibiotics, non-steroidal anti-inflammatory drugs (NSAIDs), selective serotonin reuptake inhibitors (SSRIs))
(Healthdirect 2024b)
Chronic Diarrhoea
Chronic diarrhoea may be caused by:
- Food intolerances
- Irritable bowel syndrome (IBS)
- Coeliac disease
- Cystic fibrosis
- Diabetes
- Diverticular disease
- Microscopic colitis
- Pancreatic conditions
- Bowel cancer
- Having bowel surgery
- As a side effect from chemotherapy.
(Healthdirect 2024b; Better Health Channe 2023; Gotfried 2024)
Types of Diarrhoea
Diarrhoea can be classified into different categories depending on the reason why excess fluid is present in the stool. These include:
| Type of Diarrhoea | Description | Causes |
|---|---|---|
| Reduced contact time/surface area | Occurs when the stool exits the large intestine too early, causing a watery consistency |
|
| Osmotic diarrhoea | Occurs when a substance cannot be absorbed and remains in the intestine, creating excess fluid |
|
| Secretory diarrhoea | Occurs when more fluid and salts are secreted by the bowels than can be absorbed |
|
| Inflammatory diarrhoea | Caused by inflammation of the epithelium in the large intestine, which results in proteins, blood, mucus and other fluids being released into the stool |
|
(Gotfried 2024; Jacob 2022)
Symptoms of Diarrhoea
Diarrhoea may be associated with other symptoms including:
- Nausea and vomiting
- Abdominal pain
- Fever
- Headache
- Decreased appetite
- Abdominal bloating
- Faecal urgency
- Fatigue.
(Healthdirect 2024a)
Complications of Diarrhoea
Seek medical advice if a client is experiencing:
- Bright red blood or mucus in stools
- Dark, tar-like and smelly stools (may indicate internal bleeding)
- Fever
- A large volume of watery stools
- Dehydration symptoms
- Persistent vomiting
- Difficulty keeping anything down
- Severe abdominal pain
- Weight loss
(Healthdirect 2024a, c; NHS Inform 2023)
Diarrhoea can cause excess fluid loss, which may result in dehydration (NHS Inform 2023). This has the potential to be serious, particularly in older adults and young children (Healthdirect 2024a).
Symptoms that indicate dehydration include:
- Reduced urine output
- Dark urine
- Sunken eyes
- Dry mouth and tongue
- Fatigue
- Headache
- Confusion or a change in cognition
- Rapid heartbeat
- Low blood pressure
- Muscle weakness.
(NHS Inform 2023; VIC DoH 2023)
Treating Diarrhoea

In most cases, acute diarrhoea will resolve on its own without treatment (NHS Inform 2023).
While the client recovers, you will need to manage their symptoms. You should:
- Encourage the client to get plenty of rest
- Maintain effective hygiene practices (if the diarrhoea is infection-related) to ensure that the infection does not spread
- Ensure the client stays hydrated. Consider giving water or oral rehydration fluids
- Administer medicines if clinically appropriate
- Encourage the client to eat small, light meals as soon as they feel able to
- Make short-term dietary adjustments as their intestines recover:
- Avoid giving alcohol and fatty, sweet or spicy foods
- Encourage consumption of starchy foods and yoghurt
- Manage any underlying causes (e.g. IBS, coeliac disease).
(Healthdirect 2024a; NHS Inform 2023; Better Health Channel 2023)
If the client is severely dehydrated, they may require intravenous fluid therapy (NHS Inform 2023).
If diarrhoea is a long-term issue for the client, you may need to consider dietary changes. Consult a dietician for advice and investigate any underlying causes (Continence Health Australia 2024).
Preventing Diarrhoea
The best way to prevent diarrhoea is to maintain effective hygiene practices, as this will reduce the risk of spreading infections that cause these symptoms (Healthdirect 2024a).
Refer to the following articles for comprehensive information on maintaining effective hygiene:
Test Your Knowledge
Question 1 of 3
How long does acute diarrhoea last?
Topics
Further your knowledge
 Free
Free Free
Free Free
Free Free
FreeReferences
- Better Health Channel 2023, Diarrhoea, Victoria State Government, viewed 9 April 2025, https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/diarrhoea
- Bladder & Bowel Community 2024, How The Bowel Works, Bladder & Bowel Community, viewed 9 April 2025, https://www.bladderandbowel.org/bowel/bowel-resources/how-the-bowel-works/
- Continence Health Australia 2024, Bristol Stool Chart, Continence Health Australia, viewed 9 April 2025, https://www.continence.org.au/bristol-stool-chart
- Gotfried, J 2024, Diarrhea, MSD Manual, viewed 9 April 2025, https://www.msdmanuals.com/professional/gastrointestinal-disorders/symptoms-of-gastrointestinal-disorders/diarrhea
- Healthdirect 2024a, Diarrhoea, Australian Government, viewed 9 April 2025, https://www.healthdirect.gov.au/diarrhoea
- Healthdirect 2024b, Underlying Causes of Diarrhoea, Australian Government, viewed 9 April 2025, https://www.healthdirect.gov.au/what-causes-diarrhoea
- Healthdirect 2024c, Blood in Stool, Australian Government, viewed 9 April 2025, https://www.healthdirect.gov.au/blood-in-stool
- Jacob, D 2022, What Are the 4 Types of Diarrhea?, MedicineNet, viewed 9 April 2025, https://www.medicinenet.com/what_are_the_4_types_of_diarrhea/article.htm
- MedlinePlus 2025, Diarrhea, U.S. Department of Health and Human Services, viewed 9 April 2025, https://medlineplus.gov/diarrhea.html
- Nemeth, V & Pfleghaar, N 2022, Diarrhea, StatPearls, viewed 9 April 2025, https://www.ncbi.nlm.nih.gov/books/NBK448082/
- NHS Inform 2023, Diarrhoea, NHS Scotland, viewed 9 April 2025, https://www.nhsinform.scot/illnesses-and-conditions/stomach-liver-and-gastrointestinal-tract/diarrhoea
- Victoria Department of Health 2023, Dehydration: Standardised Care Process, Victoria State Government, viewed 8 April 2025, https://www.health.vic.gov.au/residential-aged-care/standardised-care-processes
 New
New 
